Tag: weston davis

Palm Beach Equine Clinic is one of the foremost equine surgical centers in the world with three board-certified surgeons on staff, led by Dr. Weston Davis. As a busy surgeon, Dr. Davis has seen many horses with the dreaded “kissing spines” diagnosis come across his table. Two of his most interesting success stories featured horses competing in the disciplines of barrel racing and dressage.
Flossy’s Story

The words “your horse needs surgery” are ones that no horse owner wants to hear, but to Sara and Kathi Milstead, it was music to their ears. In 2016, Sara – who was 17 years old at the time and based in Loxahatchee, Florida – had been working for more than a year to find a solution to her horse’s extreme behavioral issues and chronic back pain that could not be managed. Her horse Two Blondes On Fire, a then-eight-year-old Quarter Horse mare known as “Flossy” in the barn, came into Sara’s life as a competitive barrel racer. But shortly after purchasing Flossy, Sara knew that something wasn’t right.
“We tried to do everything we could,” said Sara. “She was extremely back sore, she wasn’t holding weight, and she would try to kick your head off. We tried Regu-Mate, hormone therapy, magna wave therapy, injections, and nothing helped her. We felt that surgery was the best option instead of trying to continue injections.”
At the time, Sara and her primary veterinarian, Dr. Jordan Lewis of Palm Beach Equine Clinic (PBEC), brought Flossy to PBEC for thorough diagnostics. They determined Flossy had kissing spines.
Kissing Spines Explained
In technical terms, kissing spines are known as overriding or impinging dorsal spinous processes. The dorsal spinous process is a portion of bone extending dorsally from each vertebra. Ideally, the spinous processes are evenly spaced, allowing the horse to comfortably flex and extend its back through normal positions. With kissing spines, two or more vertebrae get too close, touch, or even overlap in places. This condition can lead to restrictions in mobility as well as severe pain, which ultimately can lead to back soreness and performance problems.
“The symptoms can be extremely broad,” acknowledged Dr. Davis. “[With] some of the horses, people will detect sensitivity when brushing over the topline. A lot of these horses get spasms in their regional musculature alongside the spinous processes.” A significant red flag is intermittent, severe bad behavior, such as kicking out, bucking, and an overall negative work attitude, something that exactly described Flossy.
Lakota’s Story

With dressage horse Lakota owned by Heidi Degele, there were minimal behavior issues, but Degele knew there had to be something more she could do to ease Lakota’s pain.
“As his age kicked in, it was like you were sitting on a two-by-four,” Heidi said of her horse’s condition. “I knew his back bothered him the most because with shockwave he felt like a different horse; he felt so supple and he had this swing in his trot, so I knew that’s what truly bothered him.” Though she could sense the stiffness and soreness as he worked, he was not one to rear, pin his ears, or refuse to work because of the pain he was feeling.
Heidi turned to Dr. Davis, who recommended a surgical route, an option he only suggests if medical treatment and physical therapy fail to improve the horse’s condition. “Not because the surgery is fraught with complications or [tends to be] unsuccessful,” he said, “but for a significant portion of these horses, if you’re really on top of the conservative measures, you may not have to opt for surgery.
“That being said, surgical interventions for kissing spines have very good success rates,” added Dr. Davis. In fact, studies have shown anywhere from 72 to 95 percent of horses return to full work after kissing spines surgery.
After Lakota made a successful recovery from his surgery in 2017, he has required no maintenance above what a typical high-level performance horse may need. Heidi attributes his success post-surgery to proper riding, including ground poles that allow him to correctly use his back, carrot stretches, and use of a massage blanket, which she has put into practice with all the horses at her farm. Dr. Davis notes that proper stretching and riding may also prolong positive effects of injections while helping horses stay more sound and supple for athletic activities.
Lakota, who went from Training Level all the way up through Grand Prix, is now used by top working students to earn medals in the Prix St. Georges, allowing them to show off their skills and earn the qualifications they need to advance their careers.

Flossy’s Turnaround
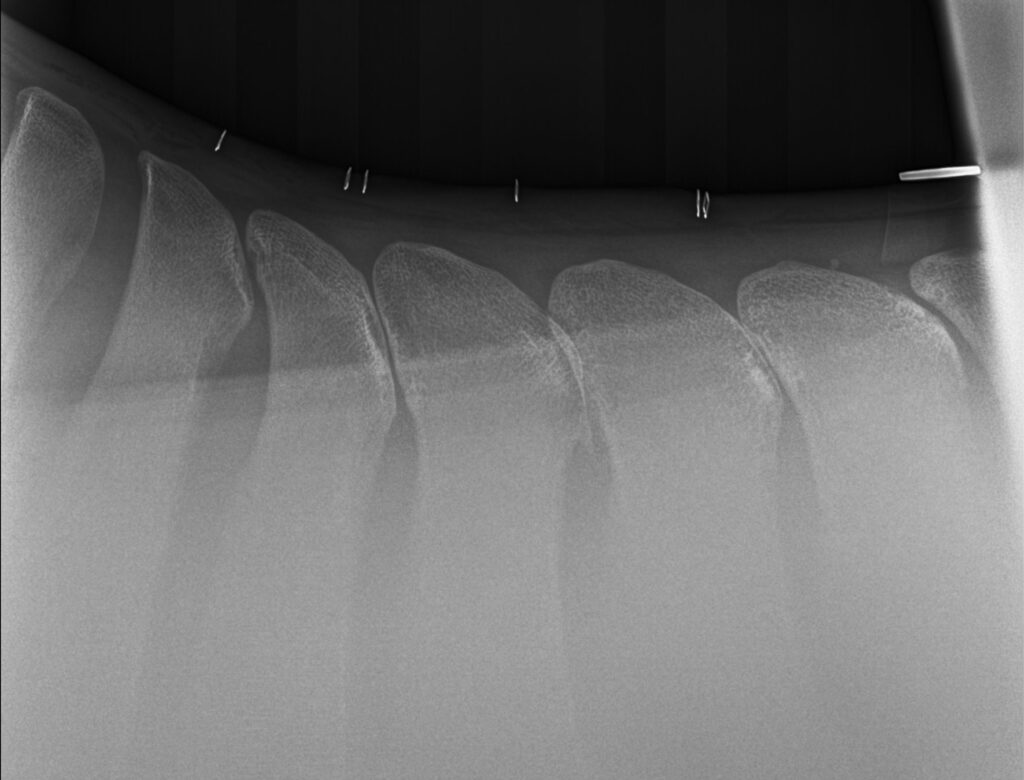
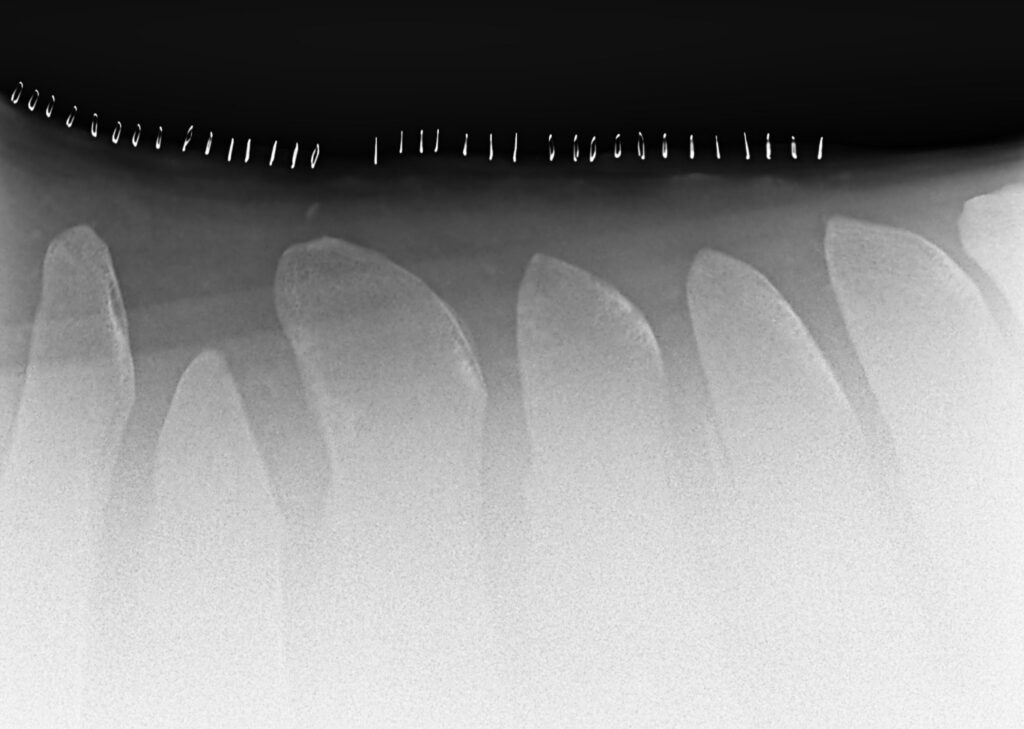
Flossy was found to have dorsal spinous process impingement at four sites in the lower thoracic vertebrae. Dr. Davis performed the surgery under general anesthesia and guided by radiographs, did a partial resection of the affected dorsal spinous processes (DSPs) to widen the spaces between adjacent DSPs and eliminate impingement.
Sara took her time bringing Flossy back to full work. Within days of the surgery, Sara saw changes in Flossy, but within six months, she was a new horse.
“Surgery was a big success,” said Sara. “Flossy went from a horse that we used to dread riding to the favorite in the barn. It broke my heart; she was just miserable. I didn’t know kissing spines existed before her diagnosis. It’s sad to think she went through that pain. She’s very much a princess, and all of her behavioral problems were because of pain. Now my three-year-old niece rides her around.”


Sara and Flossy have returned to barrel racing competition as well, now that Sara graduated from nursing school, and have placed in the money regularly including two top ten finishes out of more than 150 competitors.
“I can’t even count the number of people that I have recommended Palm Beach Equine Clinic to,” said Sara. “Everyone was really great and there was excellent communication with me through every step of her surgery and recovery.”
By finding a diagnosis for Flossy and a way to ease her pain, Sara was able to discover her diamond in the rough and go back to the competition arena with her partner for years to come.
What To Expect After the Unexpected Strikes
Featured on Horse Network
Every owner dreads having to decide whether or not to send their horse onto the surgical table for colic surgery. For a fully-informed decision, it is important that the horse’s owner or caretaker understands what to expect throughout the recovery process.
Palm Beach Equine Clinic (PBEC) veterinarian Weston Davis, DVM, DACVS, assisted by Sidney Chanutin, DVM, has an impressive success rate when it comes to colic surgeries, and the PBEC team is diligent about counseling patients’ owners on how to care for their horse post-colic surgery.

“After we determine that the patient is a strong surgical candidate, the first portion of the surgery is exploratory so we can accurately define the severity of the case,” explained Dr. Davis. “That moment is when we decide if the conditions are positive enough for us to proceed with surgery. It’s always my goal to not make a horse suffer through undue hardship if they have a poor prognosis.”
Once Dr. Davis gives the green light for surgical repair, the surgery is performed, and recovery begins immediately.
“The time period for the patient waking up in the recovery room to them standing should ideally be about 30 minutes,” continued Dr. Davis. “At PBEC, we do our best to contribute to this swift return by using a consistent anesthesia technique. Our team controls the anesthesia as lightly as we can and constantly monitors blood pressure. We administer antibiotic, anti-inflammatory, anti-endotoxic drugs, and plasma to help combat the toxins that the horse releases during colic. Our intention in the operating room is to make sure colic surgeries are completed successfully, but also in the most time-efficient manner.”
Colic surgery recovery often depends on the type and severity of the colic. At the most basic level, colic cases can be divided into two types – large intestine colic and small intestine colic – that influence the recovery procedures and outlook.
Large intestinal colic or impaction colic is characterized by the intestine folding upon itself with several changes of direction (flexures) and diameter changes. These flexures and diameter shifts can be sites for impactions, where a firm mass of feed or foreign material blocks the intestine. Impactions can be caused by coarse feeds, dehydration, or an accumulation of foreign materials such as sand.
Small intestinal colic or displacement colic can result from gas or fluid distension that results in the intestines being buoyant and subject to movement within the gut, an obstruction of the small intestine, or twisting of the gut. In general, small intestinal colics can be more difficult than large intestinal colics when it comes to recovery from surgery.
“Many people do assume that after the colic surgery is successfully completed their horse is in the clear,” said Dr. Chanutin. “However, during the first 24 to 48 hours after colic surgery, there are many factors that have to be closely monitored.
“We battle many serious endotoxic effects,” continued Dr. Chanutin. “When the colon isn’t functioning properly, microbial toxins are released inside the body. These microbials that would normally stay in the gastrointestinal tract then cause tissue damage to other bodily systems. We also need to be cognizant of the possibility of the patient developing laminitis, a disseminated intervascular coagulation (overactive clotting of the blood), or reflux, where a blockage causes fluids to back up into the stomach.”

Stages after surgery
Immediately Post-Surgery
While 30 minutes from recumbent to standing is the best-case scenario, Dr. Davis acknowledges that once that time period passes, the surgical team must intervene by encouraging the horse to get back on its feet.
Once a horse returns to its stall in the Equine Hospital at PBEC, careful monitoring begins, including physical health evaluations, bloodwork, and often, advanced imaging. According to Dr. Davis, physical exams will be conducted at least four times per day to evaluate the incision and check for any signs of fever, laminitis, lethargy, and to ensure good hydration status. An abdominal ultrasound may be done several times per day to check the health of the gut, and a tube may be passed into the stomach to check for reflux and accumulating fluid in the stomach.
“The horse must regularly be passing manure before they can be discharged,” said Dr. Chanutin. “We work toward the horse returning to a semi-normal diet before leaving PBEC. Once they are at that point, we can be fairly confident that they will not need additional monitoring or immediate attention from us.”
Returning Home
Drs. Davis and Chanutin often recommend the use of an elastic belly band to support the horse’s incision site during transport from the clinic and while recovering at home. Different types of belly bands offer varying levels of support. Some simply provide skin protection, while others are able to support the healing of the abdominal wall.

Two Weeks Post-Surgery
At the 12-to-14-day benchmark, the sutures will be removed from the horse’s incision site. The incision site is continuously checked for signs of swelling, small hernias, and infection.
At-Home Recovery
Once the horse is home, the priority is to continue monitoring the incision and return them to a normal diet if that has not already been accomplished.
The first two weeks of recovery after the horse has returned home is spent on stall rest with free-choice water and hand grazing. After this period, the horse can spend a month being turned out in a small paddock or kept in a turn-out stall. They can eventually return to full turnout during the third month. Hand-walking and grazing is permittable during all stages of the at-home recovery process. After the horse has been home for three months, the horse is likely to be approved for riding.
Generally, when a horse reaches the six-month mark in their recovery, the risk of adverse internal complications is very low, and the horse can return to full training under saddle.
When to Call the Vet?
Decreased water intake, abnormal manure output, fever, pain, or discomfort are all signals in a horse recovering from colic surgery when a veterinarian should be consulted immediately.
Long-Term Care
Dr. Davis notes that in a large number of colic surgery cases, patients that properly progress in the first two weeks after surgery will go on to make a full recovery and successfully return to their previous level of training and competition.
Depending on the specifics of the colic, however, some considerations need to be made for long-term care. For example, if the horse had sand colic, the owner would be counseled to avoid sand and offer the horse a selenium supplement to prevent a possible relapse. In large intestinal colic cases, dietary restrictions may be recommended as a prophylactic measure. Also, horses that crib can be predisposed to epiploic foramen entrapment, which is when the bowel becomes stuck in a defect in the abdomen. This could result in another colic incident, so cribbing prevention is key.
Generally, a horse that has fully recovered from colic surgery is no less healthy than it was before the colic episode. While no one wants their horse to go through colic surgery, owners can rest easy knowing that.
“A lot of people still have a negative association with colic surgery, in particular the horse’s ability to return to its intended use after surgery,” said Dr. Davis. “It’s a common old-school mentality that after a horse undergoes colic surgery, they are never going to be useful again. For us, that situation is very much the exception rather than the rule. Most, if not all, recovered colic surgery patients we treat are fortunate to return to jumping, racing, or their intended discipline.”
When the Bone Breaks
Palm Beach Equine Clinic is Changing the Prognosis for Condylar Fracture Injuries
Palm Beach Equine Clinic is changing the prognosis for condylar fracture injuries in race and sport horses. Advances in diagnostic imaging, surgical skillset, and the facilities necessary to quickly diagnose, treat, repair, and rehabilitate horses with condylar fractures have improved dramatically in recent years.

Photo by Jump Media
Most commonly seen in Thoroughbred racehorses and polo ponies, a condylar fracture was once considered a career-ending injury. Today, however, many horses fully recover and return to competing in their respective disciplines.
What is a Condylar Fracture?
A condylar fracture is a repetitive concussive injury that results in a fracture to the cannon bone above the fetlock due to large loads transmitted over the cannon bone during high-speed exercise. On a radiograph, a condylar fracture appears as a crack that goes laterally up the cannon from the fetlock joint and out the side of the bone, essentially breaking off a corner of the cannon bone, sometimes up to six inches long.

“A condylar fracture is a disease of speed,” said Dr. Robert Brusie, a surgeon at Palm Beach Equine Clinic who estimates that he repairs between 30 and 50 condylar fractures per year. “A fracture to the left lateral forelimb is most common in racehorses as they turn around the track on a weakened bone and increased loading.”

Condylar fractures are further categorized into incomplete and non-displaced (the bone fragment hasn’t broken away from the cannon bone and is still in its original position), or complete and displaced (the fragment has moved away from the cannon bone itself and can often be visible under the skin).
Additionally, condylar fractures can occur laterally or medially. According to fellow Palm Beach Equine Clinic surgeon Dr. Weston Davis, most condylar fractures tend to be lateral on the outside condyle (a rounded projection on a bone, usually for articulation with another bone similar to a knuckle or joint).
“Most lateral condylar fractures are successfully repaired,” said Dr. Davis. “Medial condylar fractures tend to be more complicated configurations because they often spiral up the leg. Those require more advanced imaging and more advanced techniques to fix.”
What is the Treatment?
The first step in effectively treating a condylar fracture through surgery is to accurately and quickly identify the problem. Board-certified radiologist Dr. Sarah Puchalski utilizes the advanced imaging services at Palm Beach Equine Clinic to accomplish exactly this.
“Stress remodeling can be detected early and easily on nuclear scintigraphy before the horse goes lame or develops a fracture,” said Dr. Puchalski. “Early diagnosis of stress remodeling allows the horse to be removed from active race training and then return to full function earlier. Early diagnosis of an actual fracture allows for repair while the fracture is small and hopefully non-displaced.”

Photo by Jump Media
Once the injury is identified as a condylar fracture, Palm Beach Equine Clinic surgeons step in to repair the fracture and start the horse on the road to recovery. Depending on surgeon preference, condylar fracture repairs can be performed with the horse under general anesthesia, or while standing under local anesthesia. During either process, surgical leg screws are used to reconnect the fractured condyle with the cannon bone.
“For a small non-displaced fracture, we would just put in one to two screws across the fracture,” explains Dr. Davis. “The technical term is to do it in ‘lag fashion,’ such that we tighten the screws down heavily and really compress the fracture line. A lot of times the fracture line is no longer visible in x-rays after it is surgically compressed. When you get that degree of compression, the fractures heal very quickly and nicely.”
More complicated fractures, or fractures that are fully displaced, may require additional screws to align the parts of the bone. For the most severe cases of condylar fractures, a locking compression plate with screws is used to stabilize and repair the bone.
Palm Beach Equine Clinic surgeon Dr. Jorge Gomez approaches a non-displaced condylar fracture while the horse is standing, which does not require general anesthesia.

“I will just sedate the horse and block above the site of the fracture,” said Dr. Gomez. “Amazingly, horses tolerate it really well. Our goal is always to have the best result for the horse, trainers, and us as veterinarians.”
According to Dr. Gomez, the recovery time required after a standing condylar fracture repair is only 90 days. This is made even easier thanks to a state-of-the-art standing surgical suite at Palm Beach Equine Clinic. The four-and-a-half-foot recessed area allows doctors to perform surgeries anywhere ventral of the carpus on front legs and hocks on hind legs from a standing position. Horses can forgo general anesthesia for a mild sedative and local nerve blocks, greatly improving surgical recovery.
“A condylar fracture was once considered the death of racehorses, and as time and science progressed, it was considered career-ending,” concluded Dr. Brusie. “Currently, veterinary medical sciences are so advanced that we have had great success with condylar fracture patients returning to full work. Luckily, with today’s advanced rehabilitation services, time, and help from mother nature, many horses can come back from an injury like this.”
When Margo Crowther of Fort Myers, FL, was looking to add a new addition to her string of barrel racing horses, she made one very important phone call. That call was to Palm Beach Equine Clinic. Dr. Weston Davis, board-certified surgeon and veterinarian at Palm Beach Equine Clinic, has been working with Crowther to keep her horses healthy, as well as performing career-saving procedures.

In 2016, Dr. Davis helped Crowther and her 2012 Quarter Horse mare Shes Packin Fame, or “Sissy,” return to the ring after what could have been a detrimental injury. Sissy suffered a rare slab fracture to the central tarsal bone in her left hock while competing in a barrel racing competition. After a diagnosis aided by Palm Beach Equine Clinic’s advanced diagnostic imaging equipment and a surgery performed by Dr. Davis, Shes Packin Fame not only returned to running barrels, but the mare was also back to winning the next year.
When Crowther found a new prospect named Grandiose Guy, or “Mater,” she turned to Dr. Davis to ensure her intended purchase would be a good fit. The Quarter Horse gelding was named the Barrel Futurities of America (BFA) Horse of the Year just after she purchased him, crowning him the top four-year-old in the country.
“When I was thinking about buying him, I called Dr. Davis and sent him videos of the horse working to review,” said Crowther, who started the purchase process late last year and chose to involve Dr. Davis in all aspects of the pre-purchase evaluation. “The horse was in Georgia, so he reviewed them from Palm Beach Equine Clinic in Wellington and gave me the stamp of approval. Once a pre-purchase was performed, I sent all the x-rays to Dr. Davis and he told me to move forward.
“I trust Dr. Davis and the team at Palm Beach Equine Clinic so much!” continued Crowther. “Barrel horses work hard and it’s so important to have a great relationship with the vet who oversees their care and knows them well in order to keep them happy and healthy.”
Regardless of breed or discipline, a pre-purchase exam involves certain steps that allow the potential owner and veterinarian to investigate the horse’s health and condition. The veterinarian gathers and interprets information by physically examining the horse’s body systems and conformation, as well as reviewing the health history. A lameness assessment is completed, including flexion tests, soft tissue structure palpation and movement evaluation. Diagnostic medical imaging tools, such as radiography, ultrasonography, endoscopy, magnetic resonance imaging, nuclear scintigraphy, or computed tomography, may be used to provide a more detailed and comprehensive profile of the horse.
Crowther purchased Mater and started running him at the beginning of last year, bringing him to the largest one-day rodeo, The American, in the Dallas Cowboys stadium in Texas in February. The competition had a $1 million payout and Mater and Crowther placed fifth.

“After so many runs, we brought him home from Texas and got him over to Dr. Davis for any maintenance work that needed to be done to keep him feeling his best,” said Crowther. “I am very picky about where I take my horses; there has to be good ground and I will not run their legs off. In conjunction with that, maintenance work with Dr. Davis is important. He performs flexion tests, utilizes the imaging at Palm Beach Equine Clinic if necessary, and makes recommendations about my horses’ health and overall well-being.”
Dr. Davis sent Mater home from Palm Beach Equine Clinic with a clean bill of health and Crowther gave the gelding a little time off before their next run. After returning to work, Mater headed to the National Barrel Horse Association (NBHA) Florida State Championships in Kissimmee.
Crowther’s diligence and Dr. Davis’ knowledge paid off when Mater won both his runs and clinched the open final at NBHA Florida State Championships. With more than 700 entries, Mater and Crowther topped them all and were crowned overall champions of the event.
“Palm Beach Equine Clinic and Dr. Davis have been a huge part of the success I have had with all of my horses,” said Crowther. “They are always there when I need them, whether I’m headed to the clinic in Wellington or they are coming to me in Fort Meyers. It’s nice to be able to know your vet will be there for you whenever you need them.”
A horse was recently admitted to Palm Beach Equine Clinic (PBEC), based in Wellington, FL, with symptoms that included bleeding from the nostril. The patient’s referring veterinarian had diagnosed the horse with an ethmoid hematoma, which in layman’s terms is essentially a mass that fills with blood in the nose or sinus cavity.
The patient was placed under the care of PBEC’s board-certified surgeon Dr. Weston Davis and Dr. Michael Myhre. They performed an airway endoscopy to locate and evaluate the hematoma that the referring veterinarian had identified. After confirming the diagnosis, Dr. Davis and Dr. Myhre were eager to ensure that it was the one and only hematoma they were battling.
Computed Tomography
PBEC is one of an elite group of equine veterinary clinics to have a computed tomography (CT) machine in their arsenal of diagnostic imaging equipment. A CT gives veterinarians a unique look at the head, neck, and spine of a horse that they would never be able to accomplish with other imaging modalities. After a CT of the patient’s sinuses, more masses were indeed identified.
“This was a fairly typical presentation of an ethmoid hematoma, but there were certainly more masses than normal,” said Dr. Myhre. “It’s for this reason that the CT was very useful. If we were not able to obtain the scans that we did, we may have missed the masses that were located deeper in the sinus.”
The cause of an ethmoid hematoma is unknown, but the mass resembles a tumor in appearance and development without being neoplastic. Horses with extensive masses may have reduced airflow and an expanding hematoma can cause pressure necrosis of the surrounding bones, but rarely causes facial distortion. Treatments of the ethmoid hematoma can range from conservative management to surgery. The conservative treatment route includes the injection of formalin – a mixture of formaldehyde gas and water – into the mass using a guarded endoscopic needle. Once injected, the mass typically regresses rapidly, but recurrence is common. For some cases, surgical excision is achieved via a frontonasal bone flap procedure.
The Approach

Due to the location and advances nature of the masses in this case, injection was not an option and the CT imaging was used to plan a surgical approach. “After sedation and a local block, we went into the sinus through a flap approach where we took a section of bone, cut it into a flap, and moved it back so we could go into the sinuses through a nice window,” said Dr. Myhre. “We removed a mass four centimeters in diameter as well as several smaller masses two to three centimeters in diameter, then flushed the area and closed.”
According to Dr. Myhre the advantages of a standing procedure included fewer risks from bleeding and fewer risks of recovering from anesthesia.
Post-surgery, the bone flap will require several weeks to heal, but the skin itself healed within one to two weeks, which is when the horse was cleared to return to normal activity.
When Margo Crowther of Fort Myers, FL, was looking to add a new addition to her string of barrel racing horses, she made one very important phone call. That first call was to Palm Beach Equine Clinic (PBEC). Dr. Weston Davis, board-certified surgeon and veterinarian at PBEC, has been working with Crowther for several years and has helped maintain her horses and even performed some career-saving procedures.
In 2016, Dr. Davis helped Crowther and her 2012 Quarter Horse mare Shes Packin Fame or “Sissy” return to the ring after what could have been a detrimental injury. Sissy suffered a rare slab fracture to the central tarsal bone in her left hock while competing in a barrel racing competition. After a diagnosis aided by PBEC’s state-of-the-art diagnostic imaging equipment and a surgery performed by Dr. Davis, Shes Packin Fame not only returned to running barrels, but the five-year-old mare was also back to winning the next year. Click here to learn more about Sissy!
Crowther Meets “Mater”
This time, Crowther turned to Dr. Davis to ensure that her intended purchase of a new horse was a good fit. When she met Grandiose Guy, known to her as “Mater,” she had to have him. The Quarter Horse gelding was named the Barrel Futurities of America (BFA) Horse of the Year just after she purchased him in 2017, crowning him the top four-year-old in the country.
“When I was thinking about buying him, I called Dr. Davis and sent him videos of the horse working to review,” said Crowther, who started the purchase process late last year. “The horse was in Georgia, so he reviewed them from PBEC in Wellington and gave me the stamp of approval. Once a pre-purchase was performed, I sent all the x-rays to Dr. Davis and he told me to move forward.
“I trust Dr. Davis and the team at PBEC so much!” continued Crowther. “Barrel horses work hard and it’s so important to have a great relationship with the veterinarian who oversees their care and knows them well in order to keep them happy and healthy.”

Crowther purchased Mater and started running him at the start of 2018, bringing him to the largest one-day rodeo, The American, in the Dallas Cowboys stadium in Texas in February. The competition had a $1 million payout and Mater and Crowther placed fifth.
“After so many runs, we brought him home from Texas and got him over to Dr. Davis for any maintenance work that needed to be done to keep him feeling his best,” said Crowther. “I am very picky about where I take my horses; there has to be good ground and I will not run their legs off. In conjunction with that, maintenance work with Dr. Davis is important. He performs flexion tests, utilizes the imaging at PBEC if necessary, and makes recommendations about my horses’ health and overall well-being.”
Dr. Davis sent Mater home from PBEC with a clean bill of health and Crowther gave the gelding a little time off before their next run. After returning to work, Mater headed to the National Barrel Horse Association (NBHA) Florida State Championships in Kissimmee in mid-June.
Success for Crowther and Mater
Crowther’s diligence and Dr. Davis’ knowledge paid off in full when Mater won both his runs and clinched the open final at NBHA Florida State Championships. With more than 700 entries, Mater and Crowther topped them all and were crowned overall champions of the event.

“PBEC and Dr. Davis have been a huge part of the success I have had with all of my horses,” said Crowther. “They are always there when I need them, whether I’m headed to the clinic or they are coming to me in Fort Meyers. It’s nice to be able to know your vet will be there for you whenever you need them.”
Palm Beach Equine Clinic (PBEC) is changing the prognosis for condylar fracture injuries among sport horses. Advances in imaging, surgical talent, and the facilities necessary to quickly diagnose, treat, repair, and rehabilitate horses with condylar fractures have recently improved immensely.
Most commonly seen in Thoroughbred racehorses and occasionally polo ponies, a condylar fracture was once considered a career-ending injury. Today, however, odds are in favor of a full recovery with horses regularly returning to competition in their respective disciplines.
What is a Condylar Fracture?

A condylar fracture is a repetitive strain injury that results in a fracture to the cannon bone above the fetlock due to large loads transmitted during high-speed exercise. 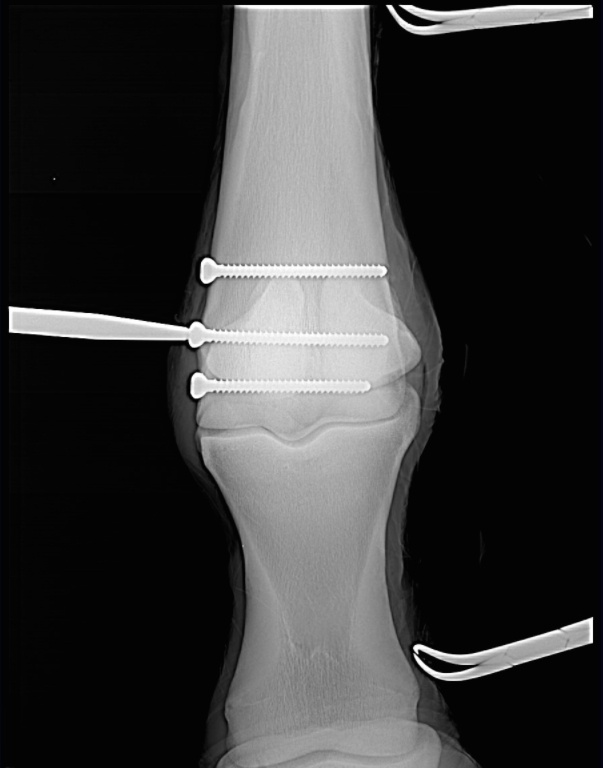
Scan showing the screws inserted during surgery (right). This patient, a Thoroughbred racehorse, walked away from surgery comfortably and is recovering well.
A condylar fracture is a repetitive strain injury that results in a fracture to the cannon bone above the fetlock due to large loads transmitted over the cannon bone during high-speed exercise. On a radiograph, a condylar fracture appears as a crack that goes laterally up the cannon from the fetlock joint and out the side of the bone, essentially breaking off a corner of the cannon bone, sometimes up to six inches long.
“A condylar fracture is a disease of speed,” said Dr. Robert Brusie, a surgeon at PBEC who estimates that he repairs between 30 and 50 condylar fractures per year. “A fracture to the left lateral forelimb is most common in racehorses as they turn around the track on a weakened bone and increased loading.”
Condylar fractures are further categorized into incomplete and non-displaced (the bone fragment hasn’t broken away from the cannon bone and is still in its original position), or complete and displaced (the fragment has moved away from the cannon bone itself and can often be visible under the skin).
Additionally, condylar fractures can occur laterally or medially. According to fellow PBEC surgeon Dr. Weston Davis, most condylar fractures tend to be lateral on the outside condyle (a rounded projection on a bone, usually for articulation with another bone similar to a knuckle or joint).
“Most lateral condylar fractures are fairly simple for us to fix,” said Dr. Davis. “Medial condylar fractures tend to be more complicated configurations because they often spiral up the leg. Those require more advanced imaging and more advanced techniques to fix.”
What is the Treatment?
The first step in effectively treating a condylar fracture through surgery is to accurately and quickly identify the problem. PBEC’s board-certified radiologist Dr. Sarah Puchalski utilizes the advanced imaging services at PBEC to accomplish exactly this.
“Stress remodeling can be detected early and easily on nuclear scintigraphy before the horse goes lame or develops a fracture,” said Dr. Puchalski. “Early diagnosis of stress remodeling allows the horse to be removed from active race training and then return to full function earlier. Early diagnosis of an actual fracture allows for repair while the fracture is small and hopefully non-displaced.”

Once the injury is identified as a condylar fracture, PBEC surgeons step in to repair the fracture and start the horse on the road to recovery. Depending on surgeon preference, condylar fracture repairs can be performed with the horse under general anesthesia, or while standing under local anesthesia. During either process, surgical leg screws are used to reconnect the fractured condyle with the cannon bone.
“For a very simple and small non-displaced fracture, we would just put in one to two screws across the fracture,” explains Dr. Davis. “The technical term is to do it in ‘lag fashion,’ such that we tighten the screws down heavily and really compress the fracture line. A lot of times the fracture line is no longer visible in x-rays after it is surgically compressed. When you get that good compression, the fractures heal very quickly and nicely.”
More complicated fractures, or fractures that are fully displaced, may require more screws to align the parts of the bone. For the most severe cases of condylar fractures, a locking compression plate with screws is used to stabilize and repair the bone.
PBEC surgeon Dr. Jorge Gomez, approaches a simpler non-displaced condylar fracture while the horse is standing, which helps to aid in a faster recovery and more successful surgical outcome.
“I will just sedate the horse and block above the site of the fracture,” said Dr. Gomez. “Amazingly, horses tolerate it really well. Our goal is always to have the best result for the horse, trainers, and us as veterinarians.”
According to Dr. Gomez, the recovery time required after a standing condylar fracture repair is only 90 days. This is made even easier thanks to a state-of-the-art surgery pit installed at PBEC. The four-and-a-half-foot recessed area allows doctors to perform surgeries on anything from a horse’s hock and below from a standing position. Horses can forgo the risks of general anesthesia for a mild sedative and local nerve blocks, greatly improving outcomes.

“A condylar fracture was once considered the death of racehorses, and as time and science progressed, it was considered career-ending,” concluded Dr. Brusie. “Currently, veterinary medical sciences are so advanced that we have had great success with condylar fracture patients returning to full work. Luckily, with today’s advanced rehabilitation services, time, and help from mother nature, many horses can come back from an injury like this.”
Success Story: Ameloblastic Fibroma
When a middle-aged mare with a mysterious mass in her mouth came under the care of Palm Beach Equine Clinic in Wellington, FL, Dr. Weston Davis pulled out all the stops to find a definitive diagnosis. The oral mass was growing at a rapid rate and was positioned just behind the bottom incisors on the left bar of the horse’s mouth.

A view of the oral mass being examined by Dr. Davis.
Computed Tomography Imaging
First, Dr. Davis turned to the use of PBEC’s state-of-the-art computed tomography (CT) machine to obtain an image of the mass and its exact location within the horse’s mouth. Then, a surgical biopsy was performed and the histopathology, or microscopic examination of the biopsied tissue, revealed the manifestation of an ameloblastic fibroma. An ameloblastic fibroma is a mixed odontogenic (dental) tumor composed of soft tissues.
“Although this tumor type rarely metastasizes, it tends to be locally invasive and aggressive, requiring the complete removal and/or aggressive radiation therapy,” said Dr. Davis, who is a board-certified surgeon at PBEC.
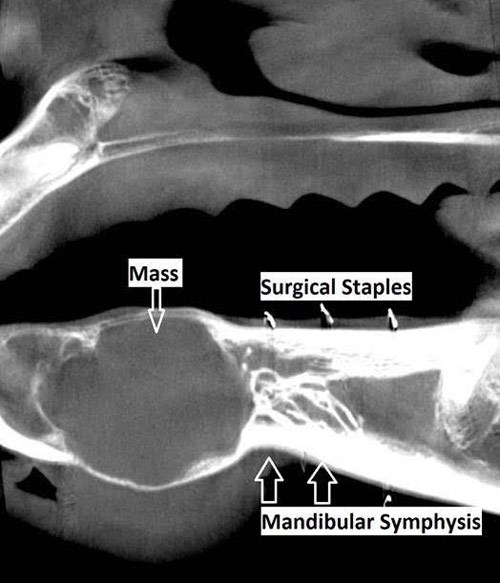
Ameloblastic Fibroma Treatment Plan
A tumor of dental origin is rarely found in humans and is extremely rare in equines, but upon diagnosis, Dr. Davis quickly identified a treatment plan, saying, “In this case, the CT mapping that was performed enabled us to completely remove the tumor via a rostral mandibulectomy with preservation of the mandibular symphysis (the joint between the two halves of the mandible).”

The horse underwent surgery at PBEC and Dr. Davis removed the tumor along with the rostral (front) mandible, which includes the lower incisor teeth and essentially the entire front portion of the lower jaw of the horse.
The obvious question that arises from a rostral mandibulectomy is “how effectively will the horse be able to eat without bottom teeth?” For this patient, however, the answer came quickly and it was nothing short of encouraging. The mare returned to eating just hours after surgery and, at her two-week checkup with Dr. Davis, was back on a normal diet of hay, grain, and – of course – treats.
According to Dr. Davis, the majority of animals that undergo this type of surgery often compensate well and have little trouble eating. For this mare, her only struggle in the future may be the prehension of very short and/or tough pasture.

A view of the lower lip of the horse after surgery. 
Two weeks post-surgery and no visible signs of a rostral mandibulectomy.
Post Mandibulectomy Surgery
Also at two weeks post-surgery, Dr. Davis approved the mare for light riding activity with a hackamore. The mare competed in the jumper ranks before surgery and at a four-week checkup, Dr. Davis gave the all-clear and the mare returned to full work. She even made a comeback in the competition ring at Palm Beach International Equestrian Center with very little visual evidence that a mandibulectomy was ever performed.
“This was a rare tumor and a rare surgery, but the horse recovered incredibly well and fast!” said Dr. Davis. “It was an excellent patient outcome. “I gave her the all-clear at four weeks post-surgery and she is already back to winning classes.”
All Photos Courtesy of Dr. Weston Davis
As sport horses become faster and stronger, veterinary medicine is often challenged to break barriers to provide the best in diagnostic and maintenance care. Palm Beach Equine Clinic is consistently on the forefront of those advances and employs a team of veterinarians equipped with the latest developments in regenerative medicine.
Two resources that have become increasingly popular to treat equine injuries are Platelet Rich Plasma (PRP) and Interleukin-1 Receptor Antagonist Protein (IRAP) to encourage regeneration of injured or degenerative tissue. Managing joint diseases and injuries using these methods is ground-breaking, but logical at their core. They essentially use naturally-occurring proteins, cells, and other natural bodily processes. Regenerative therapies put the horse’s own biological mechanisms to work stimulating healing without the use of steroids or other drugs.
What is PRP?
Platelets are among the very first cells to accumulate at an injured site, making them very important when simulating the repair process. Platelets contain granules filled with growth factors (the elements that aid in healing) and stimulate specified tissue to heal at an increased rate. To treat a horse with PRP, the veterinarians at PBEC are able to take a sample of the horse’s blood and concentrate the platelets in a high-speed centrifuge onsite. The harvest and processing procedure takes approximately 30 minutes before the concentrated platelet rich sample is injected back into the horse at the specific area of injury using sterile techniques and guided by ultrasound.

PBEC’s Board-Certified Staff Surgeon, Dr. Weston Davis, explained PRP use in more detail: “We harvest a large quantity of blood, anywhere from 60 to180 milliliters, and we process that to concentrate the segment that is very rich in platelets. We get a high concentration of platelets – we are hoping for five to eight times the concentration that you would get from normal blood. Then we take that platelet-rich extract and inject it back into an injured area to encourage a more robust healing response. Whenever you have an injury, platelets are one of the first cells that get there. They will aggregate, clump, and de-granulate. They release these granules, which are very rich in growth factors, and signal the body to start the healing process.”
What is IRAP?
IRAP is used to treat equine athletes that are susceptible to musculoskeletal injuries and osteoarthritis or degenerative joint disease. Joint trauma results in the release of inflammatory mediators such as Interleukin-1 (IL-1). IRAP uses a horse’s own anti-inflammatory protein found within the blood to counteract the destructive effects of IL-1 to slow the process of osteoarthritis. The process works by binding to the IL-1 receptors in the joint and blocking the continuation of damage and inflammation.

“We often see joint damage in sport horses because of the nature of their work, but we try to avoid overuse of steroids in joints because steroids can have long term effects on cartilage,” said PBEC veterinarian Dr. Samantha Miles. “This is a way we can manage joint disease and stop inflammation without having to consistently use steroids every time. Some of our clients will maintain their horses on IRAP alone for joint injections.”
The goal to better serve sports horses that continue to improve athletically is the driving force behind the development of even more developed and precise techniques used in regenerative medicine. And, at PBEC, the work to break new ground is never finished.
“I believe we are learning more about these technologies with more advanced science behind what they do and how they do it,” said Miles. “These treatments are natural, drug-free, and competition safe, and necessity drives the need for regenerative therapies in the sport horse world.”
Any horse owner’s worst nightmare is realized when their mount begins to show the dreaded signs of colic. For Jody Stoudenmier, a Wellington, FL, resident and avid dressage rider, she knows the symptoms all too well.

Patient History
Stoudenmier owns an 11-year-old American-bred Dutch Warmblood mare that joined her string of horses at the end of 2016 and has competed through the Intermediate II level. Sidelined by a suspensory injury last year, Beatrix was prescribed stall rest to aid in her recovery by Dr. Robert Scott of Scott Equine Services based in Ft. Lauderdale, FL. An unfortunate but common side effect of the necessary stall rest was colic. Beatrix suffered from six bouts of colic that were resolved without surgery when Dr. Scott referred Stoudenmier and Beatrix to Palm Beach Equine Clinic.
“She is such a wonderful mare; a nice mover, very athletic, sweet, sensitive, and easy to handle in the barn,” said Stoudenmier of the mare that regularly competes at the Adequan Global Dressage Festival during the winter season. “When she was recovering from her injury we tried everything to prevent her from colicking – diet, medications, hand walking – but, nothing seemed to be working.”
It was then that Palm Beach Equine Clinic’s board-certified surgeon, Dr. Weston Davis, suggested a laparoscopic surgical approach.
“Her colic had never progressed so far that we needed to do surgery before,” explained Stoudenmier. “But, at that point, I was open to anything! After speaking with Dr. Davis, I immediately had a positive feeling about it.”
Dr. Davis’ Surgical Procedure
The procedure that Dr. Davis suggested was an endoscopic ablation of nephrosplenic space. In layman’s terms, as a result of Beatrix’s colic, her colon was essentially getting caught or entrapped over the nephrosplenic ligament, which connects the left kidney to the spleen. When the colon is entrapped in this position, its contents cannot move through it and the colon becomes distended, causing the horse considerable pain, and the inevitable colic.

Dr. Davis’ solution was to close or perform an ablation of the nephrosplenic space to prevent further entrapment. The procedure can be conducted endoscopically where the horse does not have to be anesthetized, but undergoes a standing surgery with sedation and local anesthesia. A small incision is made in the left flank and the laparoscope is inserted through a smaller incision close by. The nephrosplenic space is then sutured closed so that the trough that forms the space between the kidney and spleen is obliterated and can no longer entrap the colon.
On October 9, 2017, Beatrix underwent a successful ablation of the nephrosplenic space at the hands of Dr. Davis.
“In the past, I have had several horses undergo surgery where they had to be anesthetized and it was very difficult to get them standing again after surgery,” said Stoudenmier. “We did not have that worry with Beatrix and the approach absolutely made a difference in her recovery.”
Post-Surgery Care and Recovery
Beatrix remained at Palm Beach Equine Clinic for a week and a half after surgery to jump-start her recovery before returning home to Stoudenmier, who has managed her post-surgery care with the help of both Dr. Davis and Dr. Scott.
“Dr. Davis was absolutely wonderful to work with,” said Stoudenmier of her experience at Palm Beach Equine Clinic. “He listened to my concerns, was patient, and kept his mind open.”
Dr. Davis paid a visit to Beatrix in mid-November to perform an ultrasound and together with Dr. Scott approved the mare to return to work. Stoudenmier has begun to introduce trot work into Beatrix’s routine and is optimistically expecting a full recovery, saying, “She looks super and everything looks good for the next two months. My goal by the end of the season is to get her back in the show ring!”