Category: Medical

Palm Beach Equine Clinic is one of the foremost equine surgical centers in the world with three board-certified surgeons on staff, led by Dr. Weston Davis. As a busy surgeon, Dr. Davis has seen many horses with the dreaded “kissing spines” diagnosis come across his table. Two of his most interesting success stories featured horses competing in the disciplines of barrel racing and dressage.
Flossy’s Story

The words “your horse needs surgery” are ones that no horse owner wants to hear, but to Sara and Kathi Milstead, it was music to their ears. In 2016, Sara – who was 17 years old at the time and based in Loxahatchee, Florida – had been working for more than a year to find a solution to her horse’s extreme behavioral issues and chronic back pain that could not be managed. Her horse Two Blondes On Fire, a then-eight-year-old Quarter Horse mare known as “Flossy” in the barn, came into Sara’s life as a competitive barrel racer. But shortly after purchasing Flossy, Sara knew that something wasn’t right.
“We tried to do everything we could,” said Sara. “She was extremely back sore, she wasn’t holding weight, and she would try to kick your head off. We tried Regu-Mate, hormone therapy, magna wave therapy, injections, and nothing helped her. We felt that surgery was the best option instead of trying to continue injections.”
At the time, Sara and her primary veterinarian, Dr. Jordan Lewis of Palm Beach Equine Clinic (PBEC), brought Flossy to PBEC for thorough diagnostics. They determined Flossy had kissing spines.
Kissing Spines Explained
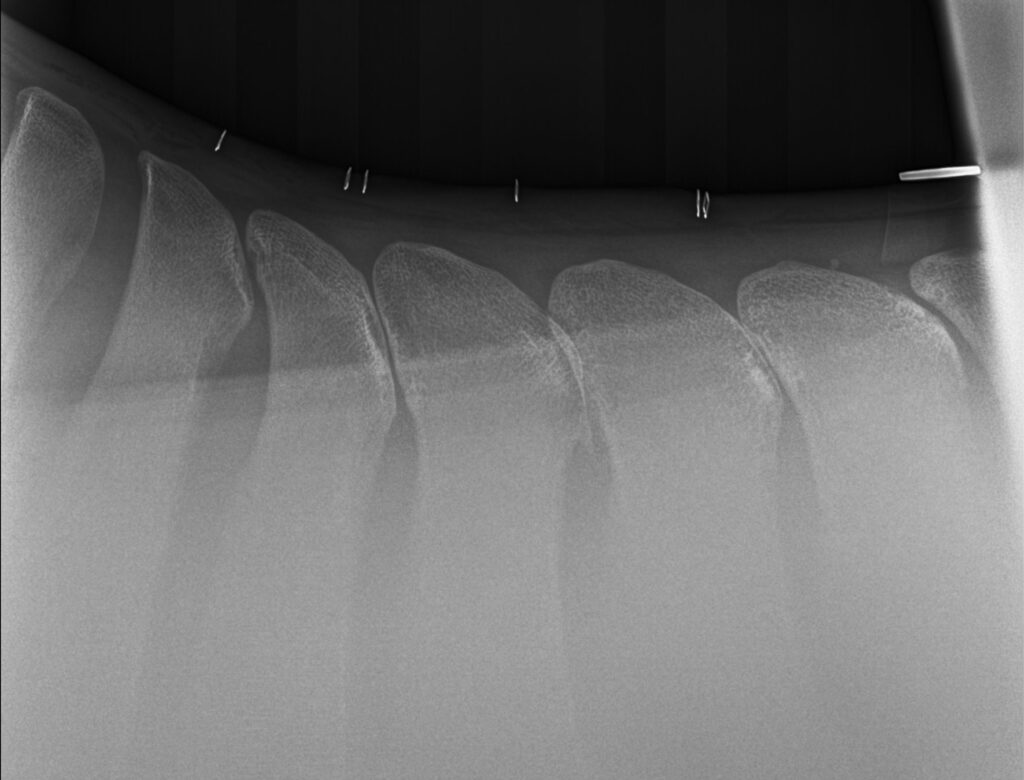
In technical terms, kissing spines are known as overriding or impinging dorsal spinous processes. The dorsal spinous process is a portion of bone extending dorsally from each vertebra. Ideally, the spinous processes are evenly spaced, allowing the horse to comfortably flex and extend its back through normal positions. With kissing spines, two or more vertebrae get too close, touch, or even overlap in places. This condition can lead to restrictions in mobility as well as severe pain, which ultimately can lead to back soreness and performance problems.
“The symptoms can be extremely broad,” acknowledged Dr. Davis. “[With] some of the horses, people will detect sensitivity when brushing over the topline. A lot of these horses get spasms in their regional musculature alongside the spinous processes.” A significant red flag is intermittent, severe bad behavior, such as kicking out, bucking, and an overall negative work attitude, something that exactly described Flossy.
Lakota’s Story

With dressage horse Lakota owned by Heidi Degele, there were minimal behavior issues, but Degele knew there had to be something more she could do to ease Lakota’s pain.
“As his age kicked in, it was like you were sitting on a two-by-four,” Heidi said of her horse’s condition. “I knew his back bothered him the most because with shockwave he felt like a different horse; he felt so supple and he had this swing in his trot, so I knew that’s what truly bothered him.” Though she could sense the stiffness and soreness as he worked, he was not one to rear, pin his ears, or refuse to work because of the pain he was feeling.
Heidi turned to Dr. Davis, who recommended a surgical route, an option he only suggests if medical treatment and physical therapy fail to improve the horse’s condition. “Not because the surgery is fraught with complications or [tends to be] unsuccessful,” he said, “but for a significant portion of these horses, if you’re really on top of the conservative measures, you may not have to opt for surgery.
“That being said, surgical interventions for kissing spines have very good success rates,” added Dr. Davis. In fact, studies have shown anywhere from 72 to 95 percent of horses return to full work after kissing spines surgery.
After Lakota made a successful recovery from his surgery in 2017, he has required no maintenance above what a typical high-level performance horse may need. Heidi attributes his success post-surgery to proper riding, including ground poles that allow him to correctly use his back, carrot stretches, and use of a massage blanket, which she has put into practice with all the horses at her farm. Dr. Davis notes that proper stretching and riding may also prolong positive effects of injections while helping horses stay more sound and supple for athletic activities.
Lakota, who went from Training Level all the way up through Grand Prix, is now used by top working students to earn medals in the Prix St. Georges, allowing them to show off their skills and earn the qualifications they need to advance their careers.

Flossy’s Turnaround
Flossy was found to have dorsal spinous process impingement at four sites in the lower thoracic vertebrae. Dr. Davis performed the surgery under general anesthesia and guided by radiographs, did a partial resection of the affected dorsal spinous processes (DSPs) to widen the spaces between adjacent DSPs and eliminate impingement.
Sara took her time bringing Flossy back to full work. Within days of the surgery, Sara saw changes in Flossy, but within six months, she was a new horse.
“Surgery was a big success,” said Sara. “Flossy went from a horse that we used to dread riding to the favorite in the barn. It broke my heart; she was just miserable. I didn’t know kissing spines existed before her diagnosis. It’s sad to think she went through that pain. She’s very much a princess, and all of her behavioral problems were because of pain. Now my three-year-old niece rides her around.”


Sara and Flossy have returned to barrel racing competition as well, now that Sara graduated from nursing school, and have placed in the money regularly including two top ten finishes out of more than 150 competitors.
“I can’t even count the number of people that I have recommended Palm Beach Equine Clinic to,” said Sara. “Everyone was really great and there was excellent communication with me through every step of her surgery and recovery.”
By finding a diagnosis for Flossy and a way to ease her pain, Sara was able to discover her diamond in the rough and go back to the competition arena with her partner for years to come.
Featured on Horse Network
In order for a racehorse to successfully speed down the track, a jumper to navigate a quick and clear round, or a dressage horse to perform a picture-perfect test, the horse must have a healthy respiratory system.
Regardless of discipline or level of training, it is key to ensure a horse is breathing properly for its overall wellbeing.
If a horse is having respiratory problems, there are several ways that a veterinarian can investigate the issue. One of the most effective tools is a dynamic endoscope, a video recording device that can be worn by the horse during exercise to observe the respiratory system while they are active.
Respiratory Specialist, Dr. David Priest of Palm Beach Equine Clinic (PBEC), focuses on upper airway diagnosis and surgery for equine athletes and often uses a dynamic endoscope to evaluate his patients.
The equine respiratory system is responsible for bringing large amounts of oxygen in and out of the lungs, where it is then used to fuel complex bodily processes. It comprises two sections, the upper and lower airways. The upper airway begins with the nostrils and extends through the larynx and into the trachea. The lower airway is made up of the lungs, which rest behind the shoulder, extend up the back, and reach toward the end of the ribcage.

Dr. David Priest
Photo by Jump Media
“Even a small decrease in lung capacity or impingement on airflow can have dramatic effects on overall health and performance,” described Dr. Priest. “Problems affecting the upper and lower airways may overlap but can include coughing or odd noises, exercise intolerance, nasal discharge, or labored breathing at rest.”
During exercise, the amount of air moved in and out of the horse increases proportionately to how hard the horse is working. The more demanding the work, the more oxygen must be used. A horse at rest inhales approximately 3.5 liters of air per second (L/s), and increases exponentially to 70 L/s at maximum exertion, according to Dr. Priest.
“If a horse is showing signs of difficulties in its respiratory health, veterinarians may use radiography or ultrasound to image the lungs,” explained Dr. Priest. “Going beyond greyscale images [such as radiographs], the veterinarian may also evaluate the upper respiratory tract through the use of an endoscope. An endoscope is a medical device with a small lens on the end that can be inserted through the horse’s nostril to view the horse’s pharynx.”

A dynamic endoscope on a harness race horse.
Photo courtesy of PBEC
If a horse is having trouble breathing only while working, it is necessary for a veterinarian to be able to evaluate them while they are active. To perform that assessment, a dynamic endoscope is used. This allows veterinarians to examine the horse’s pharynx, epiglottis, and trachea in motion. The dynamic endoscope will detect throat abnormalities and provide more information on respiratory issues or problems that are not seen when the horse is resting.
“The soft tissue structures of the horse’s upper airway experience a significant amount of force when the horse is exercising,” remarked Dr. Priest. “There is also a significant difference in resting and exercising forces, and this causes the upper airway tissues to appear anatomically normal at rest, even if they are functioning abnormally during exercise.”
A dynamic endoscope is often used with horses that have recurrent laryngeal neuropathy, commonly known as “roaring.” Recurrent laryngeal neuropathy restricts the amount of air able to reach the lungs through the horse’s upper respiratory system. This is a useful tool to diagnose the problem and also to evaluate the effectiveness of the surgery.
Respiratory difficulties during exercise can have a significant negative impact on a horse’s health and performance. A dynamic endoscope is a valuable and informative tool in Equine Sports Medicine. Once the issue is identified, there are several treatment or surgical options to address specific respiratory illness. If your horse is making an abnormal noise during exercise, or if you suspect breathing problems, contact your veterinarian to make sure your horse is performing at its best.
What To Expect After the Unexpected Strikes
Featured on Horse Network
Every owner dreads having to decide whether or not to send their horse onto the surgical table for colic surgery. For a fully-informed decision, it is important that the horse’s owner or caretaker understands what to expect throughout the recovery process.
Palm Beach Equine Clinic (PBEC) veterinarian Weston Davis, DVM, DACVS, assisted by Sidney Chanutin, DVM, has an impressive success rate when it comes to colic surgeries, and the PBEC team is diligent about counseling patients’ owners on how to care for their horse post-colic surgery.

“After we determine that the patient is a strong surgical candidate, the first portion of the surgery is exploratory so we can accurately define the severity of the case,” explained Dr. Davis. “That moment is when we decide if the conditions are positive enough for us to proceed with surgery. It’s always my goal to not make a horse suffer through undue hardship if they have a poor prognosis.”
Once Dr. Davis gives the green light for surgical repair, the surgery is performed, and recovery begins immediately.
“The time period for the patient waking up in the recovery room to them standing should ideally be about 30 minutes,” continued Dr. Davis. “At PBEC, we do our best to contribute to this swift return by using a consistent anesthesia technique. Our team controls the anesthesia as lightly as we can and constantly monitors blood pressure. We administer antibiotic, anti-inflammatory, anti-endotoxic drugs, and plasma to help combat the toxins that the horse releases during colic. Our intention in the operating room is to make sure colic surgeries are completed successfully, but also in the most time-efficient manner.”
Colic surgery recovery often depends on the type and severity of the colic. At the most basic level, colic cases can be divided into two types – large intestine colic and small intestine colic – that influence the recovery procedures and outlook.
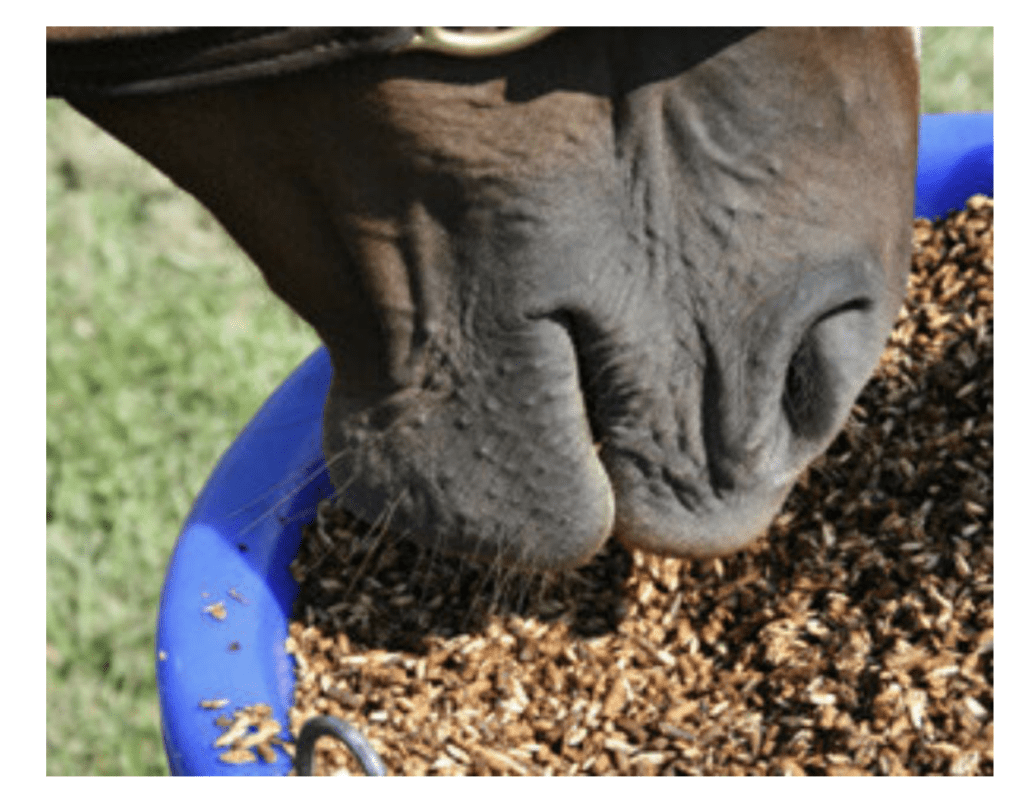
Large intestinal colic or impaction colic is characterized by the intestine folding upon itself with several changes of direction (flexures) and diameter changes. These flexures and diameter shifts can be sites for impactions, where a firm mass of feed or foreign material blocks the intestine. Impactions can be caused by coarse feeds, dehydration, or an accumulation of foreign materials such as sand.
Small intestinal colic or displacement colic can result from gas or fluid distension that results in the intestines being buoyant and subject to movement within the gut, an obstruction of the small intestine, or twisting of the gut. In general, small intestinal colics can be more difficult than large intestinal colics when it comes to recovery from surgery.
“Many people do assume that after the colic surgery is successfully completed their horse is in the clear,” said Dr. Chanutin. “However, during the first 24 to 48 hours after colic surgery, there are many factors that have to be closely monitored.
“We battle many serious endotoxic effects,” continued Dr. Chanutin. “When the colon isn’t functioning properly, microbial toxins are released inside the body. These microbials that would normally stay in the gastrointestinal tract then cause tissue damage to other bodily systems. We also need to be cognizant of the possibility of the patient developing laminitis, a disseminated intervascular coagulation (overactive clotting of the blood), or reflux, where a blockage causes fluids to back up into the stomach.”

Stages after surgery
Immediately Post-Surgery
While 30 minutes from recumbent to standing is the best-case scenario, Dr. Davis acknowledges that once that time period passes, the surgical team must intervene by encouraging the horse to get back on its feet.
Once a horse returns to its stall in the Equine Hospital at PBEC, careful monitoring begins, including physical health evaluations, bloodwork, and often, advanced imaging. According to Dr. Davis, physical exams will be conducted at least four times per day to evaluate the incision and check for any signs of fever, laminitis, lethargy, and to ensure good hydration status. An abdominal ultrasound may be done several times per day to check the health of the gut, and a tube may be passed into the stomach to check for reflux and accumulating fluid in the stomach.
“The horse must regularly be passing manure before they can be discharged,” said Dr. Chanutin. “We work toward the horse returning to a semi-normal diet before leaving PBEC. Once they are at that point, we can be fairly confident that they will not need additional monitoring or immediate attention from us.”
Returning Home
Drs. Davis and Chanutin often recommend the use of an elastic belly band to support the horse’s incision site during transport from the clinic and while recovering at home. Different types of belly bands offer varying levels of support. Some simply provide skin protection, while others are able to support the healing of the abdominal wall.

Two Weeks Post-Surgery
At the 12-to-14-day benchmark, the sutures will be removed from the horse’s incision site. The incision site is continuously checked for signs of swelling, small hernias, and infection.
At-Home Recovery
Once the horse is home, the priority is to continue monitoring the incision and return them to a normal diet if that has not already been accomplished.
The first two weeks of recovery after the horse has returned home is spent on stall rest with free-choice water and hand grazing. After this period, the horse can spend a month being turned out in a small paddock or kept in a turn-out stall. They can eventually return to full turnout during the third month. Hand-walking and grazing is permittable during all stages of the at-home recovery process. After the horse has been home for three months, the horse is likely to be approved for riding.
Generally, when a horse reaches the six-month mark in their recovery, the risk of adverse internal complications is very low, and the horse can return to full training under saddle.
When to Call the Vet?
Decreased water intake, abnormal manure output, fever, pain, or discomfort are all signals in a horse recovering from colic surgery when a veterinarian should be consulted immediately.
Long-Term Care
Dr. Davis notes that in a large number of colic surgery cases, patients that properly progress in the first two weeks after surgery will go on to make a full recovery and successfully return to their previous level of training and competition.
Depending on the specifics of the colic, however, some considerations need to be made for long-term care. For example, if the horse had sand colic, the owner would be counseled to avoid sand and offer the horse a selenium supplement to prevent a possible relapse. In large intestinal colic cases, dietary restrictions may be recommended as a prophylactic measure. Also, horses that crib can be predisposed to epiploic foramen entrapment, which is when the bowel becomes stuck in a defect in the abdomen. This could result in another colic incident, so cribbing prevention is key.
Generally, a horse that has fully recovered from colic surgery is no less healthy than it was before the colic episode. While no one wants their horse to go through colic surgery, owners can rest easy knowing that.
“A lot of people still have a negative association with colic surgery, in particular the horse’s ability to return to its intended use after surgery,” said Dr. Davis. “It’s a common old-school mentality that after a horse undergoes colic surgery, they are never going to be useful again. For us, that situation is very much the exception rather than the rule. Most, if not all, recovered colic surgery patients we treat are fortunate to return to jumping, racing, or their intended discipline.”

Dr. Marilyn Connor of Palm Beach Equine Clinic Discusses Balancing Your Horse’s Energy Sources for Performance
The modern equine athlete is asked to train and compete at far more demanding levels than horses in nature. Providing your horse with a diet that matches their metabolic needs, activity level, and training demands is key to success. To fuel our sport horses, we must first understand their nutrition and energy needs and give them the adequate support to succeed.
Physical Demands
Anaerobic vs. Aerobic Exercise

Glucose is stored in the liver and muscle cells as Glycogen, or a complex carbohydrate. Glycogen is broken down into glucose to meet metabolic energy requirements and provides energy for short to medium duration physical activity. Additionally, fat can be broken down and converted into glucose through a longer and more complex process.
Exercise can be characterized into two general categories: anaerobic and aerobic. Anaerobic exercise is characterized by short bursts of maximal effort activity, while aerobic exercise includes low to moderate intensity activity that lasts for a longer duration.
Both anaerobic and aerobic exercise utilize glucose as the primary source of fuel. Anaerobic and aerobic exercise differ in their secondary source of energy utilized once circulating glucose is depleted. Anaerobic exercise utilizes glycogen stores after glucose is depleted, while aerobic exercise is fueled by fat sources.
No equestrian sport is entirely anaerobic or aerobic. Most disciplines will have periods that require anaerobic and aerobic energy metabolism. Racehorses and western performance horses work at high intensity, fast speeds for short periods of time, requiring the body to utilize anerobic metabolism to produce energy. Show jumping and polo horses primarily use aerobic exercise yet will switch to anaerobic metabolism to keep up with energy demands of their sport. Eventing and endurance racing horses rely primarily on aerobic metabolism to support their energy needs over long periods of activity.
To support your horse during any type of sport, they must have a balanced nutrition program that sets them up for success.
Forage First

“Providing high quality forage is always my top focus for any nutrition program, regardless of the horse’s breed, age, gender, metabolic needs or athletic activity,” says Dr. Connor.
Horses are herbivores and evolved to survive by grazing on a steady supply of fresh grasses and plants. Research conducted on horses in nature shows that the average wild horse will spend 15 to 17 hours per day grazing and will travel 20 to 30 miles per day in their search for adequate food and water sources. To accommodate for the lifestyle of the modern sport horse, owners must provide high quality forage sources.
Fresh grass contains an optimal blend of key nutrients including protein, carbohydrates, vitamins and fatty acids. Once grass is cut, dried and baled as hay, the nutritional benefits begin decreasing. A week after cutting, hay loses about 60% of its vitamin A, E, and Omega 3 fatty acid content. As a general rule, horses should consume 1 to 1.5% of their body weight in hay or forage per day, with some high performing equine athletes requiring 2 to 2.5% to meet their energy needs.
When hay and forage alone are not enough to support the intense metabolic needs of the equine athlete, grain, and concentrated feed become an important part of the nutritional plan.
Building Blocks of Energy Sources
Feeding your horse with the appropriate mixture of carbohydrates, proteins, and fat is essential for fueling athletic performance.


A horse whose training requires a high level of aerobic exercise, such as a dressage horse, should receive an adequate amount of fat and carbohydrates in their diet to fuel them through longer duration training sessions by providing extended, long-lasting energy sources. Racing and barrel horses, utilizing anaerobic exercise, require a higher percentage of carbohydrates in their diets to support them through maximal effort exercise for shorter periods of time.
Carbohydrates are sourced from forage, grains, and concentrated feeds. Forage sources provide a complex source of fibrous carbohydrates that require more time for the body to digest. Concentrated feeds and grains contain starchy carbohydrates that are easily digested and quickly converted into energy to fuel a horse through intense training. A well-balanced concentrated feed will also have an appropriate blend of fat, protein, and trace minerals.
Protein is an important part of the equine diet and is found in fresh grass, dried forage, and concentrated feeds in varying amounts. Protein is made of amino acids, which are the building blocks for growth, development, repair, and maintenance of body tissues. The modern equine athlete requires a substantial amount of dietary protein to support muscle growth and ongoing tissue repair.
Fat is a key component in most equine concentrated feeds and may be supplemented by adding flax seeds, flax oil, rice bran, and corn oil. These fat sources will provide slow burning calories for sustained energy release. Fat can be especially useful for supplementing a horse’s diet when they are a “hard keeper” or if they have an underlying metabolic condition that requires dietary carbohydrates to be limited.
It is important to remember that not all fats are created equal; as some fat sources can decrease or increase inflammation in the body. Flax seed and flax seed oil are rich in anti-inflammatory omega 3 fatty acids and can be an excellent source of energy. Corn oil is commonly used to add calories and fat; however, it is a less desirable supplement due to its higher percentage of omega 6 fatty acids, which contribute to inflammation. Concentrated feeds will have varying levels of added fats depending on the type of horse it is designed to feed.
Balancing Your Horse’s Energy Sources for Performance
Whatever equestrian discipline is your passion, your horse will need to be fueled by a balanced nutritional plan.

“Feeding instructions provided on grains and concentrated feed products are designed by nutritional companies as guidelines; they are not rules and should be adjusted based on total sources of nutrition,” said Dr. Connor.
Establishing the proper balance of forage, starchy carbohydrates, fat sources, vitamins, and minerals will be different for each unique horse and the demands placed upon them.
Understanding the nutritional demands of your horse can be very simple or very intricate, depending on your unique equine athlete. When designing a feeding program, it is important take into consideration your horse’s athletic discipline, performance level, metabolic needs, stage of life, and any underlying medical conditions. Furthermore, your horse’s nutritional needs will vary over time and as they age, so it is important to periodically assess your horse’s body condition and consult with a knowledgeable veterinarian.
Speak with Dr. Marilyn Connor of Palm Beach Equine Clinic about your horse’s unique nutritional needs to ensure your horse is fully supported and on track to reach your competitive goals.
Schedule a Nutritional Consultation with Dr. Connor
Fill out the form below or call 561-793-1599 to get started.
When the Bone Breaks
Palm Beach Equine Clinic is Changing the Prognosis for Condylar Fracture Injuries
Palm Beach Equine Clinic is changing the prognosis for condylar fracture injuries in race and sport horses. Advances in diagnostic imaging, surgical skillset, and the facilities necessary to quickly diagnose, treat, repair, and rehabilitate horses with condylar fractures have improved dramatically in recent years.

Photo by Jump Media
Most commonly seen in Thoroughbred racehorses and polo ponies, a condylar fracture was once considered a career-ending injury. Today, however, many horses fully recover and return to competing in their respective disciplines.
What is a Condylar Fracture?
A condylar fracture is a repetitive concussive injury that results in a fracture to the cannon bone above the fetlock due to large loads transmitted over the cannon bone during high-speed exercise. On a radiograph, a condylar fracture appears as a crack that goes laterally up the cannon from the fetlock joint and out the side of the bone, essentially breaking off a corner of the cannon bone, sometimes up to six inches long.

“A condylar fracture is a disease of speed,” said Dr. Robert Brusie, a surgeon at Palm Beach Equine Clinic who estimates that he repairs between 30 and 50 condylar fractures per year. “A fracture to the left lateral forelimb is most common in racehorses as they turn around the track on a weakened bone and increased loading.”

Condylar fractures are further categorized into incomplete and non-displaced (the bone fragment hasn’t broken away from the cannon bone and is still in its original position), or complete and displaced (the fragment has moved away from the cannon bone itself and can often be visible under the skin).
Additionally, condylar fractures can occur laterally or medially. According to fellow Palm Beach Equine Clinic surgeon Dr. Weston Davis, most condylar fractures tend to be lateral on the outside condyle (a rounded projection on a bone, usually for articulation with another bone similar to a knuckle or joint).
“Most lateral condylar fractures are successfully repaired,” said Dr. Davis. “Medial condylar fractures tend to be more complicated configurations because they often spiral up the leg. Those require more advanced imaging and more advanced techniques to fix.”
What is the Treatment?
The first step in effectively treating a condylar fracture through surgery is to accurately and quickly identify the problem. Board-certified radiologist Dr. Sarah Puchalski utilizes the advanced imaging services at Palm Beach Equine Clinic to accomplish exactly this.
“Stress remodeling can be detected early and easily on nuclear scintigraphy before the horse goes lame or develops a fracture,” said Dr. Puchalski. “Early diagnosis of stress remodeling allows the horse to be removed from active race training and then return to full function earlier. Early diagnosis of an actual fracture allows for repair while the fracture is small and hopefully non-displaced.”

Photo by Jump Media
Once the injury is identified as a condylar fracture, Palm Beach Equine Clinic surgeons step in to repair the fracture and start the horse on the road to recovery. Depending on surgeon preference, condylar fracture repairs can be performed with the horse under general anesthesia, or while standing under local anesthesia. During either process, surgical leg screws are used to reconnect the fractured condyle with the cannon bone.
“For a small non-displaced fracture, we would just put in one to two screws across the fracture,” explains Dr. Davis. “The technical term is to do it in ‘lag fashion,’ such that we tighten the screws down heavily and really compress the fracture line. A lot of times the fracture line is no longer visible in x-rays after it is surgically compressed. When you get that degree of compression, the fractures heal very quickly and nicely.”
More complicated fractures, or fractures that are fully displaced, may require additional screws to align the parts of the bone. For the most severe cases of condylar fractures, a locking compression plate with screws is used to stabilize and repair the bone.
Palm Beach Equine Clinic surgeon Dr. Jorge Gomez approaches a non-displaced condylar fracture while the horse is standing, which does not require general anesthesia.

“I will just sedate the horse and block above the site of the fracture,” said Dr. Gomez. “Amazingly, horses tolerate it really well. Our goal is always to have the best result for the horse, trainers, and us as veterinarians.”
According to Dr. Gomez, the recovery time required after a standing condylar fracture repair is only 90 days. This is made even easier thanks to a state-of-the-art standing surgical suite at Palm Beach Equine Clinic. The four-and-a-half-foot recessed area allows doctors to perform surgeries anywhere ventral of the carpus on front legs and hocks on hind legs from a standing position. Horses can forgo general anesthesia for a mild sedative and local nerve blocks, greatly improving surgical recovery.
“A condylar fracture was once considered the death of racehorses, and as time and science progressed, it was considered career-ending,” concluded Dr. Brusie. “Currently, veterinary medical sciences are so advanced that we have had great success with condylar fracture patients returning to full work. Luckily, with today’s advanced rehabilitation services, time, and help from mother nature, many horses can come back from an injury like this.”
Horse Health Reminder: Hydration
Even in the winter months, it is important not to underestimate the heat, humidity, and sun. Palm Beach Equine Clinic stresses the importance of proper hydration and sun protection year-round, especially to Florida-based equestrians and winter season snowbirds.
There are many problems that can arise when temperatures climb, including overheating, dehydration, and colic. When the weather becomes chilly in Florida, horses often quit drinking as much water. This can lead to additional problems such as impaction. Your horse’s hydration is critically important for health and performance
Remember these 5 easy ways to protect your horse from sun and dehydration:

1. During extended periods of turnout, and when competing, horses should always have access to shaded areas. Scheduled rides and extended turnout should take place when the temperatures are lower, usually early mornings or in the evening on hot days, so the horse is not in direct sunlight.
2. The average horse drinks between five and 10 gallons of water per day. Therefore, easy and frequent access to clean, fresh water is a necessity. Pay special attention to increased intake during particularly hot days and plan accordingly.
3. Sodium in a horse’s diet is crucial for maintaining proper hydration. Providing a salt block or supplementing with properly measured electrolytes in a horse’s feed or water can help ensure that sodium requirements are being met and that your horse is drinking a sufficient amount of water.

4. Especially in the extreme summer heat, horse owners should pay attention to the amount of sweat their horse is producing. Anhidrosis, or the inability to sweat normally, can be a common challenge, particularly in hot, humid climates. In addition to lack of sweat, signs of anhidrosis can include increased respiratory rate, elevated temperature, areas of hair loss, or dry and flaky skin. If you notice any of these signs, contact Palm Beach Equine Clinic immediately.
5. Clean water buckets often and always fill with fresh water before leaving the barn. Veterinarians often recommend placing one bucket of fresh water and one bucket of electrolytes. Usually, a horse will balance his electrolytes with the opportunity to drink from one or more of these buckets.
These are just a few of the important issues to be aware of during the temperature change in Florida. Contact Palm Beach Equine Clinic to learn more about precautions that can be taken to keep horses happy and healthy throughout the winter competition season.
Typically, when a horse’s gait feels off or may be lacking usual impulsion, the rider often assumes it to be an issue of lameness associated with the forelimbs or hindlimbs. However, that may not always be the case. Utilizing advanced diagnostic imaging techniques, Palm Beach Equine Clinic is able to accurately pinpoint the specific area that is affecting overall performance. In many cases, the cervical vertebrae are often identified as the cause of lameness, asymmetry, and poor performance.
Vertebral Anatomy

The neck is composed of seven articulating cervical vertebrae running from the head to the thorax, named C1 through C7. The neck allows movement of the head while protecting the spinal cord and providing an avenue for nerves to travel. Impingement on the spinal cord and nerves connected to the cervical vertebrae can exhibit neurologically as ataxia, neck pain, or lameness.
Signs of Lameness Related to the Neck
In a lameness exam, a veterinarian will perform flexion tests and palpate areas of the body looking for decreases in the horse’s range of motion or pain upon flexion. The rider may pick up on subtle lameness issues associated with the neck by feeling a change in the horse’s suppleness or resistance to yielding in a certain direction. Lameness may even present itself as a difference in the horse’s balance, such as being heavier on the forehand, or performance issues such as late lead changes. The tried-and-true “carrot test” can also show if a horse is resistant to flexing their neck.
Identifying Lameness through Diagnostic Imaging
Historically, neck issues related to performance are generally diagnosed through a process of ruling out other areas of the body. Diagnostic imaging can now be the most powerful and effective tool for identifying the cause of lameness related to cervical injury and hereditary malformation.
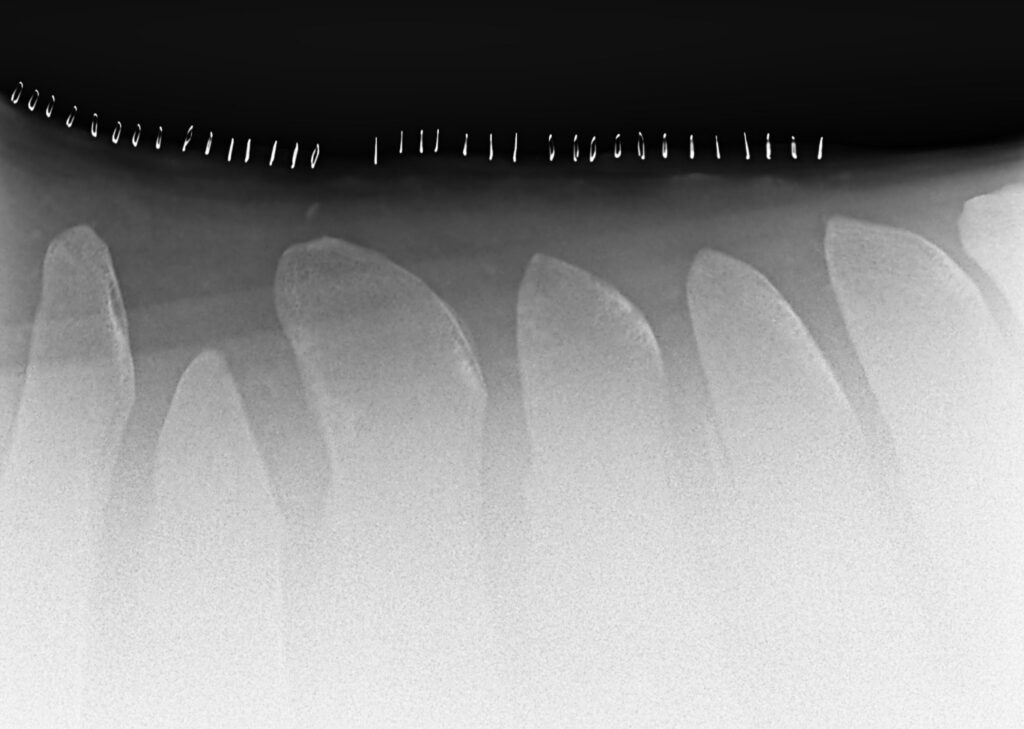
Computed Tomography (CT) scans have revolutionized the ability to assess the entire neck and can be performed while the horse is standing and under light sedation. Computed Tomography images can be rendered into three-dimensional models and sliced in any orientation, allowing the veterinarian to evaluate the vertebrae in great detail that is incomparable to standard radiographs (x-rays). These comprehensive CT scans offer veterinarians a thorough profile so they can accurately diagnose and initiate an effective response.
A standing CT scanner is the latest addition to Palm Beach Equine Clinic’s arsenal of diagnostic imaging modalities. Currently, Palm Beach Equine Clinic is the only equine hospital in South Florida offering this capability. Compared to other modalities such as MRI or Nuclear Scintigraphy, Computed Tomography offers a valuable return for its rapid acquisition of images. If you suspect there is an issue in your horse’s neck please, contact Becky at Palm Beach Equine Clinic at 561-793-1599 to schedule an appointment.
Thrush, rainrot, and scratches are problems that most equestrians have probably encountered, but in the hot, often humid summer months, these issues can incessantly plague horses and their owners. While different in their presentation, thrush, rainrot, and scratches have a lot in common. For horse owners, there are several problems that arise due to environmental factors or predisposing conditions, but these issues can easily be prevented or treated with proper care and management.
This month, Palm Beach Equine Clinic’s Dr. Bryan Dubynsky shared his expertise on the causes, treatment, and prevention of thrush, rainrot, and scratches.
Thrush
Thrush is an infection within the horse’s hoof most commonly caused by bacteria that invade the deep clefts or grooves (known as sulci) of the frog. Fusobacterium Necrophorum is the common bacterial culprit, which naturally occurs in the environment, especially in wet, muddy, or unsanitary areas. Thrush bacteria thrive where there is a lack of oxygen.
Some horses are predisposed to developing thrush due to conformation, such as a rather high heel or deep sulci, or a narrow or contracted heel. The bacteria will manifest in horse’s feet that are not picked out regularly, or standing in muddy, wet environments, including paddocks or stalls that have not been cleaned properly. Thrush can typically be first identified by the odor. The frog will have a strong, rotten odor and become spongy. Visually, the frog can even exudate (ooze) pus.
The treatment for thrush is fairly simple as it is very sensitive to oxygen. The most important thing is to have your vet or farrier trim or debride the frog to expose affected areas to the air. It is best to keep the hoof clean and dry. Adding a common detergent to the thrush areas, such as Betadine or any commercial product (Thrush Buster, Coppertox, etc.) will help to kill the bacteria. Most importantly, if the horse is not removed from those predisposing environmental factors, treatments can be ineffective.
Maintaining a level of activity for our equine partners will increase blood flow to the feet and promote health in the area. Horses found in dry environments with ample space to move typically do not suffer from thrush. The activity of horses moving keeps the frogs healthier. The more blood flow you have in the foot, the less chance there is for infection to manifest. Thrush does not always cause lameness. In extremely rare cases, thrush can penetrate deeper and cause an infection in deeper tissue or even in the coffin bone. When in doubt, always contact your veterinarian.
Rainrot (Dermotophilus Congolensis)
Rainrot is caused by a naturally occurring bacteria named Dermotophilus, which produces spores. The condition is recognized as scabby, scaly, crusty spots on areas of the horse that have been exposed to rain. It is commonly seen on the neck or across the back (dorsum). Rainrot is not typically apparent on the legs or under the belly. A surplus of rain on the skin washes away the natural protective oils. Once the skin is stripped of the natural protective layer or any sort of trauma to the skin barrier occurs, which can be even as simple as an insect bite, the Dermotophilus spores are able to invade the deeper dermis skin layers. The spores penetrate into the deeper layers of the dermis, and the body reacts by sending white blood cells and proteins to fight the invaders.
This reactive response causes small pustules, scabs, and bumps to form. Similar to thrush, rainrot is an environmental issue. It is most commonly seen in warm areas with high humidity, excess rain, and insects. The most important prevention is to keep horses out of prolonged periods of rain. A horse can be out in the rain for short periods of a day or two, but if it is constantly in hot and rainy conditions with biting insects, more than likely the horse will develop rainrot.

Dr. Dubynsky emphasizes that topical products are not worth anything if the horse is not removed from the environmental factors. Once you remove the environmental factors, a keratolytic agent (something that exfoliates keratin), such as benzoyl peroxide or an antibacterial shampoo, will help the skin heal. He also cautions that if the horse does have scabs, you do not necessarily want to pick the scabs off because then you are leaving open skin without protection for more bacteria to invade. The most important tip to healing is to keep the area dry.
In very rare, severe cases of rainrot, it is best to contact your veterinarian to put the horse on antibiotics. If left untreated, and the horse is not removed from the environmental causative factors, the infestation can lead to Staphylococcal Folliculitis; a type of Staph bacteria that will invade the hair follicles and cause a more serious situation.
Scratches
Scratches is a generic term for many different ailments. The definition of scratches can be a bacterial, fungal, or viral dermatitis or inflammatory condition of the pastern or fetlock. It is defined as a chronic Seborrheic Dermatitis, characterized by hypertrophy and exudation on the palmar plantar surface of the pastern and fetlock.
There are certainly predisposing factors for scratches, including the same environmental factors that cause thrush or rainrot. Predisposing factors for scratches include horses that are bathed often or stand in wet conditions all the time. Horses that have an excess amount of hair on their legs, especially draft horses, may be more prone to developing scratches. This is because the hair traps dirt and moisture on the skin. Scratches can develop in horses that are bathed too often, such as the intensely managed show horse. Frequent bathing of the horse can strip away the natural protective oils and barrier of the dermis. This allows bacteria or fungi to invade. When moisture penetrates the skin, it causes an inflammatory reaction. This presents as heat, redness, pain, and loss of protection to keep bacteria out.
The most effective first step for prevention and treatment should be to eliminate environmental predisposing factors. Removing excess hair during humid months and keeping horses clean and dry to the best of your ability will reduce the probability of developing an infection. Bathing horses once a day with Betadine or antifungal/antibacterial shampoo will help to clear the infection. Be sure to leave the shampoo on for 20 minutes for all of the medicine to penetrate. Rinse thoroughly, and make sure the horse is completely dry. In order to effectively treat the bacteria, horses, especially their legs, should be completely towel- or air-dried before being returned to their stalls or paddocks.
As always, contact your veterinarian immediately if there appears to be a deeper infection present, or if you would like more detailed information on how to treat and prevent these bacterial infections. To contact your Palm Beach Equine Clinic veterinarian, call 561-793-1599 or visit www.equineclinic.com.
Healthcare Reminder: Equine Summer Sores
The summer weather is here! With the humid weather, pesky flies are at their worst, which creates problems for many horse owners often leading to summer sores, medically known as Habronemiasis.
What are Summer Sores?
Summer sores are lesions on the skin caused by the larvae of equine stomach worms Habronema. These worms in the horse’s stomach produce eggs that pass through the digestive tract and are shed in the horse’s feces. Barn flies typically gather around manure and ultimately collect the parasite’s larvae on their extremities. Summer sores will occur when flies carrying the larvae deposit the eggs onto an open wound or the mucous membranes of a horse. The larvae infect the open wound or mucous membranes, causing an inflammatory reaction including symptoms of inflammation, discharge, and the production of granulation tissue infected with larvae.
Detecting Summer Sores
One way to detect a summer sore is the visible granulation of tissue containing small yellow, rice-like larvae within the skin and a mucopurulent (mucus or pus-like) discharge associated with the wound. Prevention is the most effective way of controlling summer sore outbreaks and the best way to protect horses is to implement effective methods for:

- fly control
- manure removal
- proper wound care
- an effective de-worming program
A diligent de-worming program is the most important element of prevention because effective de-wormer disrupts the parasite’s life cycle internally. The key is to kill both adult worms in the stomach and the larvae that form in the skin tissue.
Treating Summer Sores
For treatment of summer sores themselves, corticosteroids are administered to reduce the inflammatory hypersensitivity reaction, and antimicrobials treat any secondary infections that may develop as the result of an open wound. If not treated properly, summer sores can last up to several months and possibly require a costly surgical procedure to remove the granulated tissue and larvae. At the first sign of a summer sore, contact your veterinarian at Palm Beach Equine Clinic at 561-793-1599 to discuss treatment and develop an effective fly-management program for your barn.
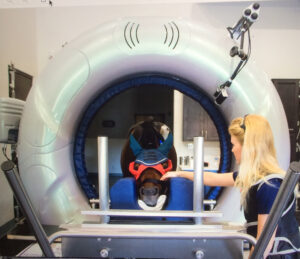
Palm Beach Equine Clinic has the most advanced state-of-the-art diagnostic imaging equipment available. More specifically, Equine Standing Magnetic Resonance Imaging (MRI) allows Palm Beach Equine Clinic to quickly and accurately diagnose injuries for their clients.

Every horse owner dreads seeing signs of lameness or discomfort in any horse, whether it is a backyard companion or a top-caliber sport horse. For performance horses, however, one of the first questions many owners ask upon contacting a veterinarian about a problem is, “Can the horse safely and comfortably return to work?” Using Palm Beach Equine Clinic’s cutting-edge equine standing MRI technology, the clinic veterinarians are best equipped to answer that question.
The equine standing MRI produces highly detailed images in several different planes to capture a complete image of the desired area. An MRI is best used to further define a specific area of bony or soft tissue that has been pinpointed as the origin of lameness. The process can be completed while the horse is in a standing position and requires only light sedation.

Lameness or performance problems are most frequently approached through routine x-rays and ultrasounds, which can come back normal. Thus, it is difficult to diagnose subtle problems because the most common tools are not sensitive enough to pick them up. At Palm Beach Equine Clinic, the Equine Standing MRI gives veterinarians an advantage when troubleshooting a lameness issue and helps them to determine a correct diagnosis in a timely manner.
Hundreds of MRIs are read each year at Palm Beach Equine Clinic. In addition to being a state-of-the-art diagnostic tool, the equine standing MRI technology also affords economic benefits to owners by having their horse’s problem diagnosed and treated safely, effectively, and quickly.