Tag: horse health

The winter show season in Wellington, FL, showcases incredible horse-and-rider partnerships across various disciplines. On one night, dressage horses will dance under the palm trees at the Adequan Global Dressage Festival – where PBEC is the official veterinarian – and the next, a field of show jumping horses will sail over massive fences.
Behind the scenes, these equine athletes have multidisciplinary teams of professionals working to keep them in top physical condition for competition. Dr. Christopher Elliott and Dr. Emma Newell of Palm Beach Equine Clinic in Wellington, FL, are key members of many of these teams, treating ailments in both dressage and jumping horses.
There are common injuries in sport horses, but typical ailments will vary between jumping and dressage horses due to the different demands of each discipline. “Dressage horses perform repetitive, collected movements that place sustained stress on the limbs and the back,” explained Dr. Elliott.
Ligament and Tendon Strains
The precise movements of dressage put stress on the soft tissues in a horse’s legs, but unlike in jumping sports, soft tissue injuries are commonly observed. Dr. Elliott pointed out, “The most common hind limb ligament injury is the proximal suspensory, and the most common tendon injury of the forelimb is the deep digital flexor tendon. These structures are loaded more for dressage horses than for jumpers, especially during collection, work transitions, and lateral movements.”
These injuries tend to present subtly and are associated with a decline in overall performance, though the rider may also notice inconsistent lameness. A loss of impulsion, difficulty maintaining collection, resistance to performing lateral movements, and other behavioral changes under saddle warrant a visit from the horse’s veterinarian.
The return to full work under saddle can be a lengthy process, beginning with straight-line exercises. The veterinarian may also suggest adjusting other aspects of the horse’s management, including reducing the intensity of the horse’s training in the future, having the horse’s saddle evaluated, improving the rider’s balance, or even reconsidering the type of footing the horse is ridden on.

The hocks are often under significant strain during collected movements.
Hock Arthritis
The hocks in a dressage horse carry a substantial load during collected work and are a common site of arthritis. The issue can be identified by stiff movement, resistance to transition or collection work, or a general decline in performance. A veterinarian will confirm this diagnosis with a thorough lameness exam, flexion tests, nerve blocks, and radiographs.
Like joint pain in jumping horses, hock arthritis in dressage horses can be treated with joint injections and anti-inflammatory medication. Reducing the difficulty or quantity of movements performed may be necessary, but regular work is usually still recommended. “Consistent, low-impact exercise is encouraged, rather than prolonged rest, with ongoing management to maintain comfort,” noted Dr. Elliott.

Diagnostic imaging may be necessary to accurately diagnose soundness issues.
Sacroiliac (SI) Pain
The sacroiliac (SI) area in the horse’s back becomes active during collected work when a horse engages its hind end, tilts its pelvis, and brings its hind legs underneath its body. A horse experiencing discomfort in this area may struggle with flying lead changes and exhibit uneven hind-end engagement, reduced impulsion, or behavioral changes under saddle.
“Diagnosing these issues can be challenging and often involves ruling out other sources of hind-end lameness,” admitted Dr. Elliott, adding that diagnostic block and advanced imaging may be necessary to evaluate the horse.
Targeted SI joint injections can improve comfort, while physical therapy exercises aimed at strengthening the horse’s hind end and core muscles are often part of the long-term management plan for the horse.
The Secret to Success
Riders and caretakers play a significant role in maintaining their horses’ health and well-being. Early recognition of subtle lameness signs is essential, and Dr. Newell emphasized, “Knowing your horse and knowing their nuances, I think, is what’s really going to keep our equine athletes in work longer.”
With a full suite of diagnostic equipment and an expert team of veterinarians, PBEC is fully equipped to provide equine patients with a high standard of care. “A highlight of being a veterinarian at PBEC is the ability to conduct a CT, a bone scan, or a standing MRI. We can provide clients in-depth imaging with a quick turnaround on results with the amount of technology we have here at PBEC,” shared Dr. Newell. She also noted that radiographs and ultrasounds can be conducted in the field, eliminating the need to visit the clinic.
Whether your goal is to trot down the centerline at Adequan Global Dressage Festival or make the jump-off at the Winter Equestrian Festival, Palm Beach Equine Clinic is dedicated to helping your horse perform their best. Visit www.EquineClinic.com for more information or call 561-793-1599 to make an appointment.

From inside the dressage boards to the jumping arena, the risk of injury for equine athletes always exists. Dr. Christopher Elliott and Dr. Emma Newell of Palm Beach Equine Clinic in Wellington, FL, explained that some riding activities are more closely associated with specific injuries. “The physical demands of each discipline place stress on very different parts of the horse’s body,” noted Dr. Elliott.
In the sport of jumping, the concussive forces of takeoff and landing put strain on the horse’s legs. Joints and soft tissues, such as tendons and ligaments, are designed to absorb this shock, but excessive and repetitive force on these structures can cause problems. Suspensory ligaments, flexor tendons, and joints are three areas Dr. Elliott commonly treats for injuries in jumping horses.
Suspensory Ligaments
The suspensory ligament can become injured through repetitive strain. A lameness exam, nerve blocks, and an ultrasound are used to determine the location and severity of the injury. Clinical signs of a suspensory injury can vary from subtle or intermittent lameness, reluctance to jump, or, potentially, a gradual decline in performance. Overt and persistent lameness can be seen in more significant injuries.
Rest and a controlled exercise rehabilitation program are the cornerstones of treatment. Additional therapies include shockwave and platelet-rich plasma (PRP), which may further support healing.
Dr. Newell reminds horse owners that rehabilitation is tailored to each horse and begins with ground exercises before gradually progressing to ridden work over the course of several months. Regular veterinary check-ups are essential for monitoring progress and making adjustments to the treatment as needed.

PRP Injections
Flexor Tendons: The DDFT
Flexor tendons, specifically the Deep Digital Flexor Tendon (DDFT), are another common site of injury in jumping horses.
Injury to the DDFT in the jumping horse typically occurs within the hoof capsule. Horses will present with varying degrees of lameness that are eliminated by distal limb nerve blocks. An MRI is required for definitive diagnosis of injury to the DDFT within the hoof.
A horse with this injury will likely be prescribed rest, controlled exercise rehabilitation, and corrective shoeing, with return to previous levels of performance typically being seen between nine and 12 months.

Dr. Santiago Demierre performing a flexion test
Photo courtesy of Jump Media
Joint Pain: Inflammation and Arthritis
Osteoarthritis is one of the most common ailments in competition horses, especially jumping horses. Nearly all of a jumping horses’ distal limb joints undergo repeated strain throughout the course of their careers, with the stifles, hocks, and forelimb coffin joints being common sites of inflammation.
If joint inflammation is suspected, the horse’s veterinarian will conduct a physical evaluation, including limb palpation, watching the horse trot in hand, and often also under saddle. Flexion tests are frequently performed along with nerve blocks and radiographs, if necessary, to pinpoint the area of concern.
Managing osteoarthritis is complex and should be tailored to each horse. Veterinary treatment of joint inflammation typically includes targeted joint injections, either with corticosteroids or biological agents. Other systemic treatments involve nutraceutical supplements (oral and injectable), judicious use of systemic anti-inflammatories, and other targeted complementary therapies.
By paying close attention, owners and riders can detect ailments early, giving their horse the best chance at sustained performance. Dr. Newell advised, “Knowing your horse is the best way to prevent these types of injuries. Working closely with your veterinarian to continually evaluate a horse is the key to success.”
To keep your horse on the right track, contact Palm Beach Equine Clinic at 561-793-1599.
By Lindsay Berreth / Jump Media
With modern veterinary technology, there are several ways to breed your treasured mare should she have trouble getting pregnant or carrying a foal. Intracytoplasmic sperm injection, or ICSI, an alternative to traditional embryo transfer is becoming a popular option for the sport horse mare.

According to Dr. Justin McNaughten BVMS, DACT, the equine reproductive specialist at Palm Beach Equine Clinic (PBEC) in Wellington, FL, the ICSI procedure was originally developed to help overcome subfertility in mares and stallions. The first ICSI foal was born in 1996, and since then the procedure has gained popularity amongst breeders for mare and stallion owners alike.
Before ICSI, many breeders’ options for their mare were limited to embryo transfer, which involves breeding the donor mare, flushing the donor mare’s uterus, and then transferring the embryo into a recipient mare that has been synchronized to the donor mare’s cycle. For stallions with limited semen reserves, there wasn’t much that could be done. However, ICSI has become an invaluable tool for preserving sperm from deceased stallions or stallions with limited semen availability as the procedure uses less sperm to fertilize an egg.
A significant advantage of ICSI for sport horse mares, compared to traditional embryo transfer, is that the procedure can be performed at any stage of the estrous cycle, regardless of the natural breeding season. This flexibility allows mares to concentrate on their competition schedules and minimizes disruptions to their training or show commitments.
During the procedure, oocytes, or eggs, are collected from a donor mare’s follicles on the ovary. “It is a valuable option for mares with uterine, oviductal, or cervical disorders that would not allow the mare to be an embryo donor,” said Dr. McNaughten. The ICSI procedure bypasses most of the reproductive tract and goes straight to the source for the oocytes (shown below), the ovary.

Palm Beach Equine Clinic offers the first stage of the procedure, the oocyte aspiration or egg retrieval. Vets will ship the eggs to an ICSI lab to complete the maturation and fertilization processes. During aspiration, mares are sedated and restrained in stocks. The veterinarian passes a long handle ultrasound probe which also houses the aspiration needle into the mare’s vagina. The ovary is stabilized by the veterinarian per rectum to allow for visualization of the ovary and the follicle. The needle is inserted into the follicle; the fluid is aspirated, the wall of the follicle is scraped, then the follicle is flushed and the fluid is aspirated. The scrapping, flushing, and aspirating are repeated multiple times to help dislodge the immature oocyte. The flush fluid that is recovered is then filtered, and any oocytes that are recovered are prepared and transferred into a special holding and shipped off for the next step. The entire process is known as transvaginal oocyte aspiration (TVA) in the US or ovum pick-up (OPU) in other parts of the world.
While the procedure is becoming more routine, it does carry some risks. To safeguard against any risks the procedure is only performed at the clinic. All mares are provided pain relief during the procedure and the following day. “We recommend that mares stay overnight at the clinic to be monitored for any signs of discomfort,” noted Dr. McNaughten, “and most mares return to full work within the week following the procedure.”

Once an ICSI lab receives the egg or eggs, they are put into a maturation media and monitored for 24 hours. “The eggs that we’re taking from the mare are immature, they’re incubated in a specialized maturation media,” said Dr. McNaughten. Each oocyte that matures, is then fertilized with a single sperm cell. “That’s the process of the intracytoplasmic sperm injection or ICSI. If all goes well, the fertilized oocytes are monitored to see if there’s any cellular division or cleavage, which means that fertilization was successful. Those will be monitored for the next 7-10 days until they reach the blastocyst or embryo stage.”
Maturation, fertilization, and embryo production rates can be affected by numerous factors including bred, age, season, level of work, semen quality and whether it is cool shipped or frozen semen. On average 50 to 60% of eggs will mature and be suitable for fertilization. Intracytoplasmic sperm injection laboratories report 70 to 80% of oocytes fertilized typically divide and grow, and 20 to 30% of fertilized oocytes will grow in culture to the blastocyst stage for embryo transfer. The final step in the ICSI process is to transfer the embryo to a recipient mare or freeze it. According to Dr. McNaughten, 60 to 70% of transfers are successful.
In our hands ICSI has become an invaluable tool for in vitro produced embryos not only on the mare side but for select valuable stallions. “To put it into perspective, in a conventional frozen semen breeding dose, the minimum dose is 250 million progressively motile sperm for one breeding. With ICSI, one sperm is used to fertilize one egg,” he explained. “We have also been very successful in producing embryos and foals using frozen semen from a deceased stallions that previously had not produced embryos through conventional breeding management with the same frozen semen.”

Palm Beach Equine Clinic is here to help you achieve your breeding goals. Our veterinarians specialize in breeding and reproduction and utilize the latest technology to ensure a seamless experience for both you and your mare. Contact us today at 561-793-1599 to schedule an appointment or to learn more.
A recent popular post on PBEC’s social media was about retired Davie County, FL, police horse Charlie, who injured himself in true equine fashion – spectacularly and with no one knowing how – during the night while turned out in a field. Charlie was adopted by the mother of one of the Davie County police officers who also works for the Sheriff’s Department. They brought Charlie to PBEC to repair a large laceration on his side.

Dr. Michelle Maguire was on hand to care for Charlie and explained the steps it took to get him back to healing. Dr. Maguire and her team administered intravenous sedation in order to repair with him standing up then injected local anesthesia around the circumference of the laceration, which measured approximately 12 by 18 inches.
“This case was particularly challenging because it was a very large area with multiple flaps and went through many layers, including skin, subcutaneous tissue, and the muscle layers overlying the thorax,” said Dr. Maguire. “Luckily there was no penetration into the thoracic cavity.”
Dr. Maguire used walking sutures to close the laceration, extending from the skin flap’s deep dermis to the underlying fascia of the body wall. This approach helps eliminate
dead space to help prevent seroma formation and infection, reduce skin tension, promote wound closure, and lower the risk of dehiscence, a surgical complication where a wound ruptures along the incision after surgery.
Because the skin can’t handle tension, you can’t just suture the skin itself. Dr. Maguire also used a Jackson Pratt drain, a commonly used surgical drain that provides a constant, low suction to pull fluid from a surgical incision site to decrease swelling and reduce the risk of infection. The drain consists of a thin, rubber tube and a soft, round squeeze bulb, or “grenade” on the end that maintains negative pressure and allows for an active drainage system.

Dr. Maguire noted that Charlie’s prognosis is very good, and he is expected to make a full recovery. He has been doing well at home, and the wound has held together without dehiscence.
She added, “The aftercare protocol was a course of systemic antibiotics and anti-inflammatories, along with maintaining a compressive for the first two weeks postoperatively until skin sutures were removed.
“The horse handled everything very well,” she continued. “He was in pain the first day postoperatively, but as the inflammation subsided, he was a normal happy horse.”
The team at Palm Beach Equine Clinic is happy to report that Charlie is back home grazing. While he will have a scar, it won’t affect his quality of life, and he will have quite a story to tell his friends!
Fernando J. Marqués, DVM, Diplomate ACVIM, Diplomate ACVSMR

The exceptional athletic abilities of horses can be attributed to several factors, including physiological adaptations, some of which are influenced by training. Muscles, and all cells in the body, require energy to function. Energy from food (carbohydrates, fats, and proteins) is not directly transferred to muscles for biological work. Instead, it is converted into an energy-rich substance known as ATP. The oxidation of carbohydrates, fats, and proteins is the process that produces ATP. There are three main energy systems that supply ATP to the cells: the immediate energy system, the short-term energy system, and the long-term energy system.
The immediate energy system relies on high-energy phosphate sources and plays a crucial role during intense physical activities of short duration that require immediate fuel. These high-energy phosphates are quickly depleted, typically within 20 to 30 seconds of maximum exertion, similar to what happens in humans.
The short-term energy system generates ATP mainly from stored muscle carbohydrates called glycogen. This process does not require oxygen, which is why it is referred to as anaerobic metabolism, leading to lactate accumulation within the muscle cells.
The long-term energy system, or aerobic system, produces ATP during prolonged, intense physical activity. This process requires oxygen, hence the name aerobic metabolism. In this system, fats are a significant fuel source.
The contribution of each energy system and fuel source (carbohydrates, fats, and to a lesser extent proteins) varies depending on factors such as exercise intensity and duration, training status, muscle fiber composition, and oxygen supply to the muscles. Understanding these factors is crucial, as exercise is generally categorized into aerobic/endurance (low intensity over a long duration) and power/strength (high intensity over a short duration). In practice, pure endurance or pure strength activities are rare, and most sports combine elements of both.
Additionally, muscles adapt to specific exercises and sports, which triggers the development of particular muscle fibers that utilize different fuel sources and energy systems to produce ATP.
In equestrian sports, no discipline is exclusively anaerobic or aerobic. Most sports require a combination of both energy systems. For example, racehorses and western performance horses engage in high-intensity, fast-paced activities for short periods, primarily relying on anaerobic metabolism. Conversely, show jumping and polo horses mainly engage in aerobic exercise but switch to anaerobic metabolism to meet the intense energy demands of their sport. Eventing and endurance racing horses, on the other hand, rely predominantly on aerobic metabolism to sustain their energy levels over prolonged periods of activity.
Designing an effective training program for a horse requires considering the optimal adaptation of muscle fiber composition to enhance metabolic function and improve performance in the specific sport.
References:
- Hinchcliff K., Geor R., Kaneps A. Equine Exercise Physiology- The Science of Exercise in the Athletic Horse. Saunders
- McArdle W., Katch F., Katch V. Exercise Physiology. Wolters Kluwer, 8th Edition.
- https://equineclinic.com/medical/understanding-energy-support-for-the-performance-horse/
By Alice Collins / Jump Media
The warm late summer of 2024 has paved the way for more mosquitos and heralded the start of West Nile Virus (WNV) and Eastern Equine Encephalitis (EEE) season for both horses and humans. WNV and EEE are both equine encephalitis viruses spread by infected mosquitos. They can cause severe brain inflammation and neurological issues in humans and horses and can be fatal in unvaccinated or under-vaccinated equine populations.
With almost daily cases of WNV in horses being reported in several U.S. states throughout August 2024, plus news of humans contracting the rare but extremely serious EEE virus, people are rightfully concerned about how to protect their animals and themselves from both WNV and EEE. The Wellington, Florida-based Palm Beach Equine Center (PBEC)advises on what you can do to minimize the risk of exposure and infection.

WNV and EEE by the Numbers
Both WNV and EEE circulate in the environment between mosquitoes and birds and are spread to horses and humans by the bite of an infected mosquito. However, even though they get sick, humans and horses are dead-end hosts that do not, in turn, spread these viruses back to mosquitoes that bite them.
Since 1999, more than 27,600 U.S. horses have been confirmed to have WNV, with an estimated fatality rate of 30-40%. With yearly activity of around 300 equine cases in the U.S., WNV is now considered endemic, persisting at a consistent level with fairly predictable rates of infection and spread.
EEE, also known as sleeping sickness, causes inflammation of the brain and spinal cord. Mortality can exceed 90% in unvaccinated horses and is lower in horses with partial protection or previous vaccination. Death usually occurs within two to three days of the onset of signs. Horses that survive may have permanent neurologic deficits.
While the diseases sound alarming, the good news is that vaccination is a very effective barrier for your horse. EEE and WNV inoculations are considered core vaccines by the American Association of Equine Practitioners. Annual injections for all horses, preferably in the spring before mosquito season, are strongly recommended. Initial vaccination is followed in four to six weeks with a booster, with yearly revaccination thereafter. Horses living in areas with mosquitos year-round may need EEE vaccinations two or three times a year for full protection.
Clinical Signs
The clinical signs of the two illnesses are almost identical, and can include:
- Depression and anorexia without fever when initially infected
- Mild low-grade fever in about 25% of affected horses with WVN
- Moderate to high fever in horses with EEE
- Lack of appetite
- Lethargy/drowsiness
- Neurologic signs, the onset of which are frequently sudden and progressive
- Periods of hyperexcitability, apprehension and/or drowsiness
- Fine tremors of the face and neck muscles
- Cranial nerve paralysis — facial paralysis and weakness of the tongue are very common
- Head tilt, droopy lip, muzzle deviation
- Weakness, ataxia, and lack of coordination in one or more limbs
- Complete paralysis of one or more limbs
- Colic
- Inability to stand
Diagnosis and Treatment
A veterinarian will diagnose both WNV and EEE by testing the horse’s serum, a component of whole blood. There is no cure for either virus, but horses showing clinical signs are given supportive care.
Prevention
Aside from vigilant vaccination suitable for the horse’s environment, there are other measures owners can take to prevent infection from both WNV and EEE. They include frequent use of insect repellent, which should be reapplied after rain, keeping horses stabled at night, minimizing standing water, and eliminating areas in which water can collect, such as leaf piles or old tires.
PBEC President Dr. Scott Swerdlin advises, “We can vaccinate against all these diseases, and it’s really important to remember that it’s not just the first set; it takes at least two injections for the horse to develop immunity.”
Swerdlin also points out that horses traveling into an affected region can be put at far greater risk, adding, “People who bring horses to the U.S. from South America or Europe are exposing them to different diseases than they are accustomed to in their native country. They should vaccinate the horses immediately on arrival and then, after the first vaccine, every 12 months. In Florida, where there is a huge mosquito population, we recommend vaccinating against EEE and WNV, as well as rhinovirus, every six months for maximum protection.”
There are no approved human vaccines for WNV or EEE. Personal protective measures include using mosquito repellents, wearing long-sleeved shirts tucked into long pants, and limiting time outdoors from dusk to dawn. Using air conditioning and installing screens further decreases the risk of exposure.
For additional questions, veterinary assistance, or to book your horse’s vaccinations, call Palm Beach Equine Clinic at 561-793-1599.
What To Expect After the Unexpected Strikes
Featured on Horse Network
Every owner dreads having to decide whether or not to send their horse onto the surgical table for colic surgery. For a fully-informed decision, it is important that the horse’s owner or caretaker understands what to expect throughout the recovery process.
Palm Beach Equine Clinic (PBEC) veterinarian Weston Davis, DVM, DACVS, assisted by Sidney Chanutin, DVM, has an impressive success rate when it comes to colic surgeries, and the PBEC team is diligent about counseling patients’ owners on how to care for their horse post-colic surgery.

“After we determine that the patient is a strong surgical candidate, the first portion of the surgery is exploratory so we can accurately define the severity of the case,” explained Dr. Davis. “That moment is when we decide if the conditions are positive enough for us to proceed with surgery. It’s always my goal to not make a horse suffer through undue hardship if they have a poor prognosis.”
Once Dr. Davis gives the green light for surgical repair, the surgery is performed, and recovery begins immediately.
“The time period for the patient waking up in the recovery room to them standing should ideally be about 30 minutes,” continued Dr. Davis. “At PBEC, we do our best to contribute to this swift return by using a consistent anesthesia technique. Our team controls the anesthesia as lightly as we can and constantly monitors blood pressure. We administer antibiotic, anti-inflammatory, anti-endotoxic drugs, and plasma to help combat the toxins that the horse releases during colic. Our intention in the operating room is to make sure colic surgeries are completed successfully, but also in the most time-efficient manner.”
Colic surgery recovery often depends on the type and severity of the colic. At the most basic level, colic cases can be divided into two types – large intestine colic and small intestine colic – that influence the recovery procedures and outlook.
Large intestinal colic or impaction colic is characterized by the intestine folding upon itself with several changes of direction (flexures) and diameter changes. These flexures and diameter shifts can be sites for impactions, where a firm mass of feed or foreign material blocks the intestine. Impactions can be caused by coarse feeds, dehydration, or an accumulation of foreign materials such as sand.
Small intestinal colic or displacement colic can result from gas or fluid distension that results in the intestines being buoyant and subject to movement within the gut, an obstruction of the small intestine, or twisting of the gut. In general, small intestinal colics can be more difficult than large intestinal colics when it comes to recovery from surgery.
“Many people do assume that after the colic surgery is successfully completed their horse is in the clear,” said Dr. Chanutin. “However, during the first 24 to 48 hours after colic surgery, there are many factors that have to be closely monitored.
“We battle many serious endotoxic effects,” continued Dr. Chanutin. “When the colon isn’t functioning properly, microbial toxins are released inside the body. These microbials that would normally stay in the gastrointestinal tract then cause tissue damage to other bodily systems. We also need to be cognizant of the possibility of the patient developing laminitis, a disseminated intervascular coagulation (overactive clotting of the blood), or reflux, where a blockage causes fluids to back up into the stomach.”

Stages after surgery
Immediately Post-Surgery
While 30 minutes from recumbent to standing is the best-case scenario, Dr. Davis acknowledges that once that time period passes, the surgical team must intervene by encouraging the horse to get back on its feet.
Once a horse returns to its stall in the Equine Hospital at PBEC, careful monitoring begins, including physical health evaluations, bloodwork, and often, advanced imaging. According to Dr. Davis, physical exams will be conducted at least four times per day to evaluate the incision and check for any signs of fever, laminitis, lethargy, and to ensure good hydration status. An abdominal ultrasound may be done several times per day to check the health of the gut, and a tube may be passed into the stomach to check for reflux and accumulating fluid in the stomach.
“The horse must regularly be passing manure before they can be discharged,” said Dr. Chanutin. “We work toward the horse returning to a semi-normal diet before leaving PBEC. Once they are at that point, we can be fairly confident that they will not need additional monitoring or immediate attention from us.”
Returning Home
Drs. Davis and Chanutin often recommend the use of an elastic belly band to support the horse’s incision site during transport from the clinic and while recovering at home. Different types of belly bands offer varying levels of support. Some simply provide skin protection, while others are able to support the healing of the abdominal wall.

Two Weeks Post-Surgery
At the 12-to-14-day benchmark, the sutures will be removed from the horse’s incision site. The incision site is continuously checked for signs of swelling, small hernias, and infection.
At-Home Recovery
Once the horse is home, the priority is to continue monitoring the incision and return them to a normal diet if that has not already been accomplished.
The first two weeks of recovery after the horse has returned home is spent on stall rest with free-choice water and hand grazing. After this period, the horse can spend a month being turned out in a small paddock or kept in a turn-out stall. They can eventually return to full turnout during the third month. Hand-walking and grazing is permittable during all stages of the at-home recovery process. After the horse has been home for three months, the horse is likely to be approved for riding.
Generally, when a horse reaches the six-month mark in their recovery, the risk of adverse internal complications is very low, and the horse can return to full training under saddle.
When to Call the Vet?
Decreased water intake, abnormal manure output, fever, pain, or discomfort are all signals in a horse recovering from colic surgery when a veterinarian should be consulted immediately.
Long-Term Care
Dr. Davis notes that in a large number of colic surgery cases, patients that properly progress in the first two weeks after surgery will go on to make a full recovery and successfully return to their previous level of training and competition.
Depending on the specifics of the colic, however, some considerations need to be made for long-term care. For example, if the horse had sand colic, the owner would be counseled to avoid sand and offer the horse a selenium supplement to prevent a possible relapse. In large intestinal colic cases, dietary restrictions may be recommended as a prophylactic measure. Also, horses that crib can be predisposed to epiploic foramen entrapment, which is when the bowel becomes stuck in a defect in the abdomen. This could result in another colic incident, so cribbing prevention is key.
Generally, a horse that has fully recovered from colic surgery is no less healthy than it was before the colic episode. While no one wants their horse to go through colic surgery, owners can rest easy knowing that.
“A lot of people still have a negative association with colic surgery, in particular the horse’s ability to return to its intended use after surgery,” said Dr. Davis. “It’s a common old-school mentality that after a horse undergoes colic surgery, they are never going to be useful again. For us, that situation is very much the exception rather than the rule. Most, if not all, recovered colic surgery patients we treat are fortunate to return to jumping, racing, or their intended discipline.”

Dr. Marilyn Connor of Palm Beach Equine Clinic Discusses Balancing Your Horse’s Energy Sources for Performance
The modern equine athlete is asked to train and compete at far more demanding levels than horses in nature. Providing your horse with a diet that matches their metabolic needs, activity level, and training demands is key to success. To fuel our sport horses, we must first understand their nutrition and energy needs and give them the adequate support to succeed.
Physical Demands
Anaerobic vs. Aerobic Exercise

Glucose is stored in the liver and muscle cells as Glycogen, or a complex carbohydrate. Glycogen is broken down into glucose to meet metabolic energy requirements and provides energy for short to medium duration physical activity. Additionally, fat can be broken down and converted into glucose through a longer and more complex process.
Exercise can be characterized into two general categories: anaerobic and aerobic. Anaerobic exercise is characterized by short bursts of maximal effort activity, while aerobic exercise includes low to moderate intensity activity that lasts for a longer duration.
Both anaerobic and aerobic exercise utilize glucose as the primary source of fuel. Anaerobic and aerobic exercise differ in their secondary source of energy utilized once circulating glucose is depleted. Anaerobic exercise utilizes glycogen stores after glucose is depleted, while aerobic exercise is fueled by fat sources.
No equestrian sport is entirely anaerobic or aerobic. Most disciplines will have periods that require anaerobic and aerobic energy metabolism. Racehorses and western performance horses work at high intensity, fast speeds for short periods of time, requiring the body to utilize anerobic metabolism to produce energy. Show jumping and polo horses primarily use aerobic exercise yet will switch to anaerobic metabolism to keep up with energy demands of their sport. Eventing and endurance racing horses rely primarily on aerobic metabolism to support their energy needs over long periods of activity.
To support your horse during any type of sport, they must have a balanced nutrition program that sets them up for success.
Forage First

“Providing high quality forage is always my top focus for any nutrition program, regardless of the horse’s breed, age, gender, metabolic needs or athletic activity,” says Dr. Connor.
Horses are herbivores and evolved to survive by grazing on a steady supply of fresh grasses and plants. Research conducted on horses in nature shows that the average wild horse will spend 15 to 17 hours per day grazing and will travel 20 to 30 miles per day in their search for adequate food and water sources. To accommodate for the lifestyle of the modern sport horse, owners must provide high quality forage sources.
Fresh grass contains an optimal blend of key nutrients including protein, carbohydrates, vitamins and fatty acids. Once grass is cut, dried and baled as hay, the nutritional benefits begin decreasing. A week after cutting, hay loses about 60% of its vitamin A, E, and Omega 3 fatty acid content. As a general rule, horses should consume 1 to 1.5% of their body weight in hay or forage per day, with some high performing equine athletes requiring 2 to 2.5% to meet their energy needs.
When hay and forage alone are not enough to support the intense metabolic needs of the equine athlete, grain, and concentrated feed become an important part of the nutritional plan.
Building Blocks of Energy Sources
Feeding your horse with the appropriate mixture of carbohydrates, proteins, and fat is essential for fueling athletic performance.


A horse whose training requires a high level of aerobic exercise, such as a dressage horse, should receive an adequate amount of fat and carbohydrates in their diet to fuel them through longer duration training sessions by providing extended, long-lasting energy sources. Racing and barrel horses, utilizing anaerobic exercise, require a higher percentage of carbohydrates in their diets to support them through maximal effort exercise for shorter periods of time.
Carbohydrates are sourced from forage, grains, and concentrated feeds. Forage sources provide a complex source of fibrous carbohydrates that require more time for the body to digest. Concentrated feeds and grains contain starchy carbohydrates that are easily digested and quickly converted into energy to fuel a horse through intense training. A well-balanced concentrated feed will also have an appropriate blend of fat, protein, and trace minerals.
Protein is an important part of the equine diet and is found in fresh grass, dried forage, and concentrated feeds in varying amounts. Protein is made of amino acids, which are the building blocks for growth, development, repair, and maintenance of body tissues. The modern equine athlete requires a substantial amount of dietary protein to support muscle growth and ongoing tissue repair.
Fat is a key component in most equine concentrated feeds and may be supplemented by adding flax seeds, flax oil, rice bran, and corn oil. These fat sources will provide slow burning calories for sustained energy release. Fat can be especially useful for supplementing a horse’s diet when they are a “hard keeper” or if they have an underlying metabolic condition that requires dietary carbohydrates to be limited.
It is important to remember that not all fats are created equal; as some fat sources can decrease or increase inflammation in the body. Flax seed and flax seed oil are rich in anti-inflammatory omega 3 fatty acids and can be an excellent source of energy. Corn oil is commonly used to add calories and fat; however, it is a less desirable supplement due to its higher percentage of omega 6 fatty acids, which contribute to inflammation. Concentrated feeds will have varying levels of added fats depending on the type of horse it is designed to feed.
Balancing Your Horse’s Energy Sources for Performance
Whatever equestrian discipline is your passion, your horse will need to be fueled by a balanced nutritional plan.

“Feeding instructions provided on grains and concentrated feed products are designed by nutritional companies as guidelines; they are not rules and should be adjusted based on total sources of nutrition,” said Dr. Connor.
Establishing the proper balance of forage, starchy carbohydrates, fat sources, vitamins, and minerals will be different for each unique horse and the demands placed upon them.
Understanding the nutritional demands of your horse can be very simple or very intricate, depending on your unique equine athlete. When designing a feeding program, it is important take into consideration your horse’s athletic discipline, performance level, metabolic needs, stage of life, and any underlying medical conditions. Furthermore, your horse’s nutritional needs will vary over time and as they age, so it is important to periodically assess your horse’s body condition and consult with a knowledgeable veterinarian.
Speak with Dr. Marilyn Connor of Palm Beach Equine Clinic about your horse’s unique nutritional needs to ensure your horse is fully supported and on track to reach your competitive goals.
Schedule a Nutritional Consultation with Dr. Connor
Fill out the form below or call 561-793-1599 to get started.
Horse Health Reminder: Hydration
Even in the winter months, it is important not to underestimate the heat, humidity, and sun. Palm Beach Equine Clinic stresses the importance of proper hydration and sun protection year-round, especially to Florida-based equestrians and winter season snowbirds.
There are many problems that can arise when temperatures climb, including overheating, dehydration, and colic. When the weather becomes chilly in Florida, horses often quit drinking as much water. This can lead to additional problems such as impaction. Your horse’s hydration is critically important for health and performance
Remember these 5 easy ways to protect your horse from sun and dehydration:

1. During extended periods of turnout, and when competing, horses should always have access to shaded areas. Scheduled rides and extended turnout should take place when the temperatures are lower, usually early mornings or in the evening on hot days, so the horse is not in direct sunlight.
2. The average horse drinks between five and 10 gallons of water per day. Therefore, easy and frequent access to clean, fresh water is a necessity. Pay special attention to increased intake during particularly hot days and plan accordingly.
3. Sodium in a horse’s diet is crucial for maintaining proper hydration. Providing a salt block or supplementing with properly measured electrolytes in a horse’s feed or water can help ensure that sodium requirements are being met and that your horse is drinking a sufficient amount of water.

4. Especially in the extreme summer heat, horse owners should pay attention to the amount of sweat their horse is producing. Anhidrosis, or the inability to sweat normally, can be a common challenge, particularly in hot, humid climates. In addition to lack of sweat, signs of anhidrosis can include increased respiratory rate, elevated temperature, areas of hair loss, or dry and flaky skin. If you notice any of these signs, contact Palm Beach Equine Clinic immediately.
5. Clean water buckets often and always fill with fresh water before leaving the barn. Veterinarians often recommend placing one bucket of fresh water and one bucket of electrolytes. Usually, a horse will balance his electrolytes with the opportunity to drink from one or more of these buckets.
These are just a few of the important issues to be aware of during the temperature change in Florida. Contact Palm Beach Equine Clinic to learn more about precautions that can be taken to keep horses happy and healthy throughout the winter competition season.
Thrush, rainrot, and scratches are problems that most equestrians have probably encountered, but in the hot, often humid summer months, these issues can incessantly plague horses and their owners. While different in their presentation, thrush, rainrot, and scratches have a lot in common. For horse owners, there are several problems that arise due to environmental factors or predisposing conditions, but these issues can easily be prevented or treated with proper care and management.
This month, Palm Beach Equine Clinic’s Dr. Bryan Dubynsky shared his expertise on the causes, treatment, and prevention of thrush, rainrot, and scratches.
Thrush
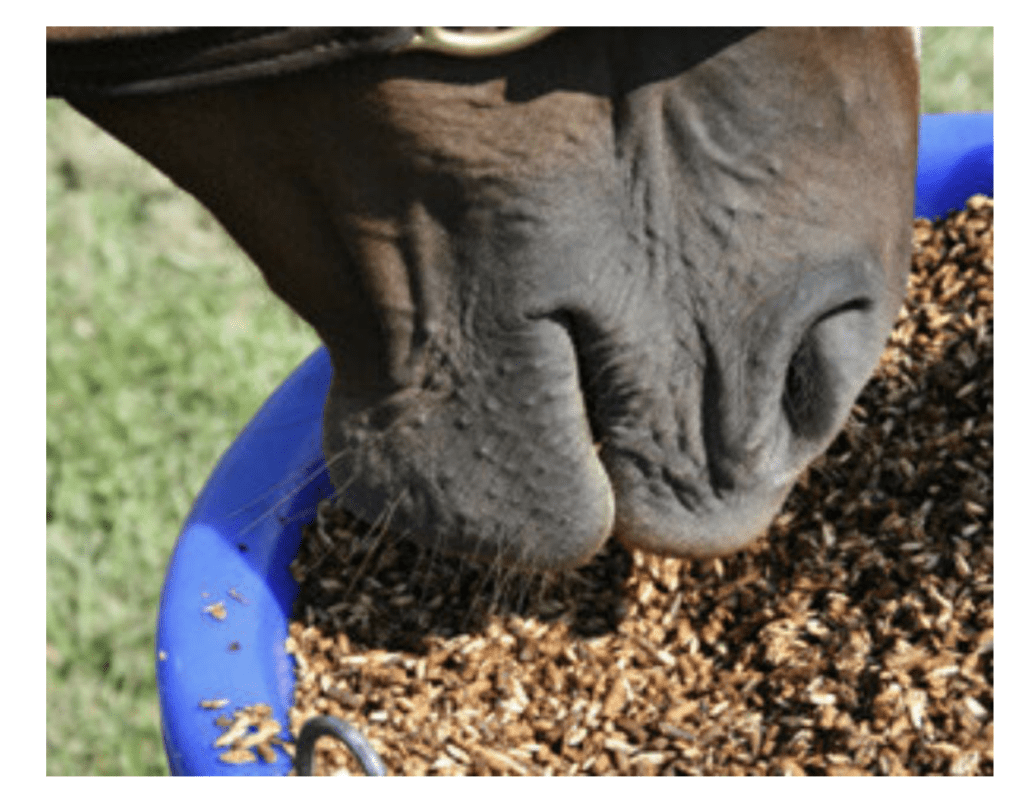
Thrush is an infection within the horse’s hoof most commonly caused by bacteria that invade the deep clefts or grooves (known as sulci) of the frog. Fusobacterium Necrophorum is the common bacterial culprit, which naturally occurs in the environment, especially in wet, muddy, or unsanitary areas. Thrush bacteria thrive where there is a lack of oxygen.
Some horses are predisposed to developing thrush due to conformation, such as a rather high heel or deep sulci, or a narrow or contracted heel. The bacteria will manifest in horse’s feet that are not picked out regularly, or standing in muddy, wet environments, including paddocks or stalls that have not been cleaned properly. Thrush can typically be first identified by the odor. The frog will have a strong, rotten odor and become spongy. Visually, the frog can even exudate (ooze) pus.
The treatment for thrush is fairly simple as it is very sensitive to oxygen. The most important thing is to have your vet or farrier trim or debride the frog to expose affected areas to the air. It is best to keep the hoof clean and dry. Adding a common detergent to the thrush areas, such as Betadine or any commercial product (Thrush Buster, Coppertox, etc.) will help to kill the bacteria. Most importantly, if the horse is not removed from those predisposing environmental factors, treatments can be ineffective.
Maintaining a level of activity for our equine partners will increase blood flow to the feet and promote health in the area. Horses found in dry environments with ample space to move typically do not suffer from thrush. The activity of horses moving keeps the frogs healthier. The more blood flow you have in the foot, the less chance there is for infection to manifest. Thrush does not always cause lameness. In extremely rare cases, thrush can penetrate deeper and cause an infection in deeper tissue or even in the coffin bone. When in doubt, always contact your veterinarian.
Rainrot (Dermotophilus Congolensis)
Rainrot is caused by a naturally occurring bacteria named Dermotophilus, which produces spores. The condition is recognized as scabby, scaly, crusty spots on areas of the horse that have been exposed to rain. It is commonly seen on the neck or across the back (dorsum). Rainrot is not typically apparent on the legs or under the belly. A surplus of rain on the skin washes away the natural protective oils. Once the skin is stripped of the natural protective layer or any sort of trauma to the skin barrier occurs, which can be even as simple as an insect bite, the Dermotophilus spores are able to invade the deeper dermis skin layers. The spores penetrate into the deeper layers of the dermis, and the body reacts by sending white blood cells and proteins to fight the invaders.
This reactive response causes small pustules, scabs, and bumps to form. Similar to thrush, rainrot is an environmental issue. It is most commonly seen in warm areas with high humidity, excess rain, and insects. The most important prevention is to keep horses out of prolonged periods of rain. A horse can be out in the rain for short periods of a day or two, but if it is constantly in hot and rainy conditions with biting insects, more than likely the horse will develop rainrot.

Dr. Dubynsky emphasizes that topical products are not worth anything if the horse is not removed from the environmental factors. Once you remove the environmental factors, a keratolytic agent (something that exfoliates keratin), such as benzoyl peroxide or an antibacterial shampoo, will help the skin heal. He also cautions that if the horse does have scabs, you do not necessarily want to pick the scabs off because then you are leaving open skin without protection for more bacteria to invade. The most important tip to healing is to keep the area dry.
In very rare, severe cases of rainrot, it is best to contact your veterinarian to put the horse on antibiotics. If left untreated, and the horse is not removed from the environmental causative factors, the infestation can lead to Staphylococcal Folliculitis; a type of Staph bacteria that will invade the hair follicles and cause a more serious situation.
Scratches
Scratches is a generic term for many different ailments. The definition of scratches can be a bacterial, fungal, or viral dermatitis or inflammatory condition of the pastern or fetlock. It is defined as a chronic Seborrheic Dermatitis, characterized by hypertrophy and exudation on the palmar plantar surface of the pastern and fetlock.
There are certainly predisposing factors for scratches, including the same environmental factors that cause thrush or rainrot. Predisposing factors for scratches include horses that are bathed often or stand in wet conditions all the time. Horses that have an excess amount of hair on their legs, especially draft horses, may be more prone to developing scratches. This is because the hair traps dirt and moisture on the skin. Scratches can develop in horses that are bathed too often, such as the intensely managed show horse. Frequent bathing of the horse can strip away the natural protective oils and barrier of the dermis. This allows bacteria or fungi to invade. When moisture penetrates the skin, it causes an inflammatory reaction. This presents as heat, redness, pain, and loss of protection to keep bacteria out.
The most effective first step for prevention and treatment should be to eliminate environmental predisposing factors. Removing excess hair during humid months and keeping horses clean and dry to the best of your ability will reduce the probability of developing an infection. Bathing horses once a day with Betadine or antifungal/antibacterial shampoo will help to clear the infection. Be sure to leave the shampoo on for 20 minutes for all of the medicine to penetrate. Rinse thoroughly, and make sure the horse is completely dry. In order to effectively treat the bacteria, horses, especially their legs, should be completely towel- or air-dried before being returned to their stalls or paddocks.
As always, contact your veterinarian immediately if there appears to be a deeper infection present, or if you would like more detailed information on how to treat and prevent these bacterial infections. To contact your Palm Beach Equine Clinic veterinarian, call 561-793-1599 or visit www.equineclinic.com.