At Palm Beach Equine Clinic in Wellington, FL, the team of Board-Certified surgeons are experts in minimally invasive surgical techniques, aiming to reduce joint disease, resolve lameness, and improve the longevity of sport horse careers.

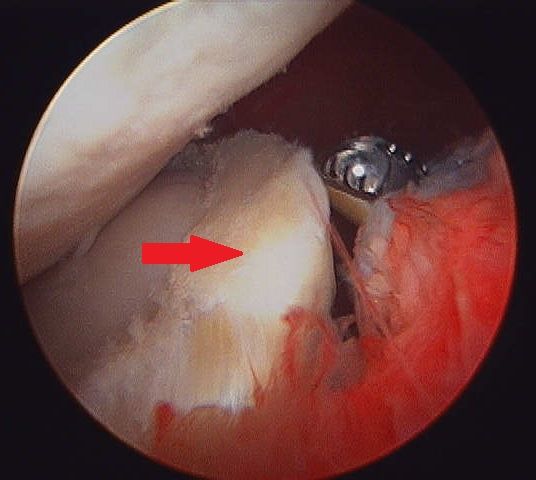
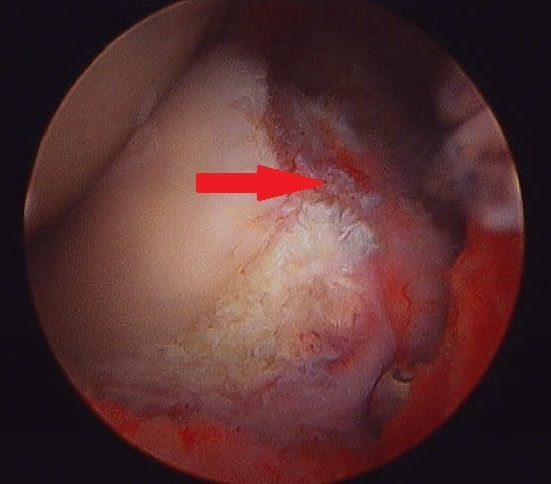
Arthroscopy (or arthroscopic surgery) is a minimally invasive surgical technique that can be performed on an injured joint or synovial structure to accurately explore and treat pathology. The surgery generally involves two very small (8mm) keyhole incisions. The first incision is where the surgeon will insert the arthroscope, which is an instrument with a small surgical grade camera installed that allows a complete, clear view of the interior joint surface. The second small incision is created to insert the surgical instrument to perform the procedure.
Arthroscopy is used to treat a broad range of injuries inside of a joint. Chip fracture removal is a procedure that is particularly commonly in both young Warmblood horses with developmental disease and in racehorses travelling at high speeds. A small chip fracture can cause persistent irritation in the joint as well as arthritis if left untreated. It is best removed immediately so that no further damage is created. The surgeon can go into the joint, remove the chip, and clean up the surrounding cartilage. Most horses recovery quickly and return to their normal athletic activity.
Board-Certified Surgeon Dr. Weston Davis performs many arthroscopic surgeries at Palm Beach Equine Clinic alongside fellow surgeons Dr. Robert Brusie and Dr. Jorge Gomez.
“In many horses, we consider arthroscopy as a prophylactic measure, intervening after injury, but before the development of a generalized degenerative arthritic cycle ensues,” Dr. Davis stated. “Arthroscopy is definitely something that you want to do early in the game if you feel like the horse has joint disease, or a chip, or cartilage disease, or an undefined injury that is not responding appropriately to medical therapy. Arthroscopy can be curative for some of these horses. But if you do not intervene early on in the course of the disease and there is already advanced arthritis, then you have missed your window.
“Arthroscopy is a preferred treatment because it is minimally invasive so most horses can go right back to work,” Dr. Davis continued. “In a typical scenario, we thoroughly explore the joint with the arthroscopic camera, we remove a chip or repair a lesion, and the horse is not lame after the surgery. Because of the small incisions, there is minimal aftercare and horses are often able to go back to work quickly.”
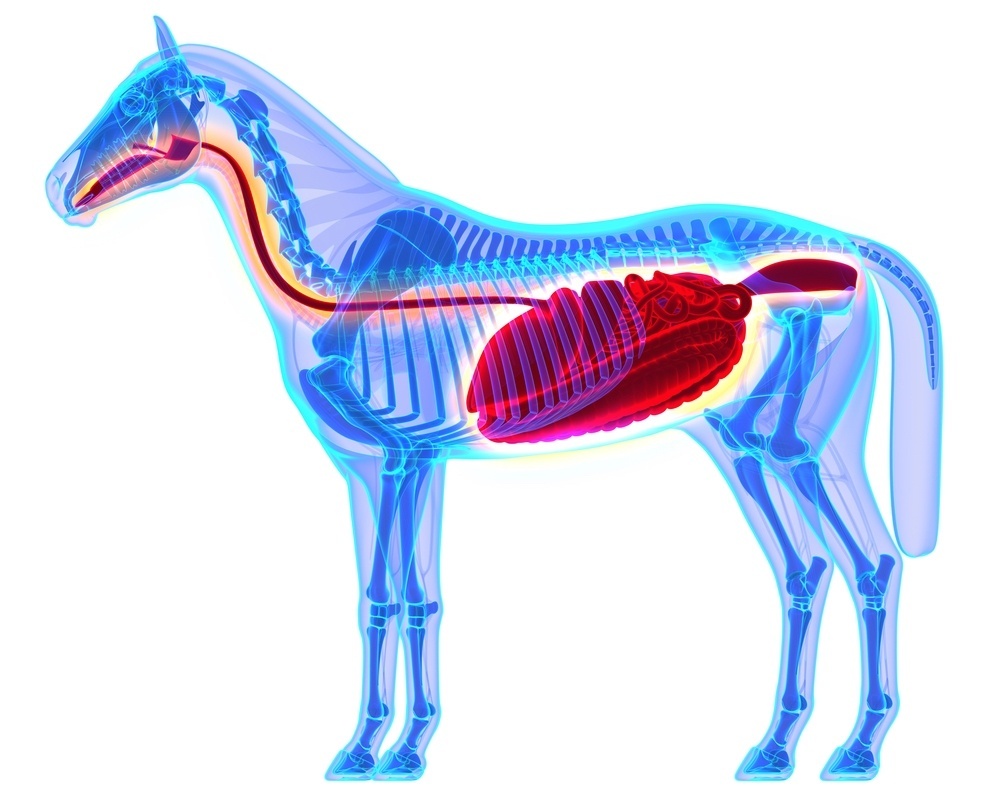
Other common indications for arthroscopic surgery are meniscal disease in the stifle, subchondral cystic lesions, primary cartilage lesions, and debridement of damaged tendinous/ligamentous tissue (such as deep digital flexor tendon tears in the navicular bursa). The surgeons at Palm Beach Equine Clinic can perform arthroscopy on virtually any joint in the horse. Anything from the Temporomandibular Joint (TMJ) of the head to the navicular bursa within the hoof capsule can be explored and treated with this minimally invasive approach.
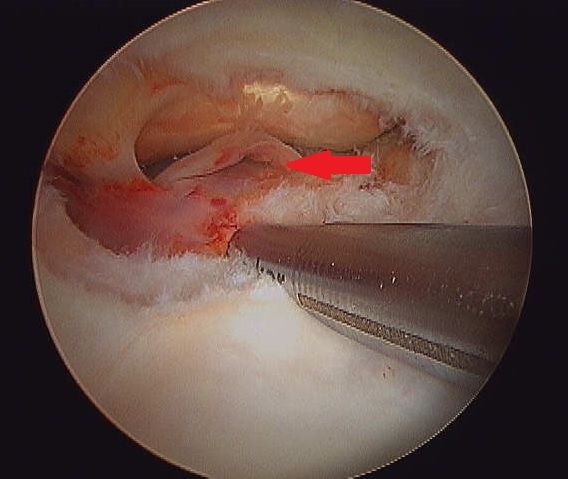

Almost all arthroscopies are performed under general anesthesia with the horse on its back. New renovations at Palm Beach Equine Clinic include a set of stocks of adjustable height adjacent to a surgeon’s pit, allowing the surgeons to have eye-level access to the joint they are working on, enabling many new procedures on the legs of standing horses.
Minimally invasive surgery allows for a simple and quick recovery for the horse. The traditional horse would be on stall rest with a bandage on until the sutures come out at two weeks, and then start doing some light hand walking and physical therapy. Barring severe damage in the joint or associated tendon/ligament disruption, most cases will undergo a six-week rest and rehabilitation protocol, then return to normal work.
As always, the advanced diagnostic imaging at Palm Beach Equine Clinic permits the surgeons to get a complete evaluation of an injury involving a joint to ensure the best possible outcome. Depending on the injury type, digital radiographs, ultrasound, MRI, and Nuclear Scintigraphy, or a combination thereof, may be used for pre-operative diagnosis and planning. Ultrasound and digital radiography are available for intra-operative use. Intra-operative CT scanning will also be available in the future with the new additions at Palm Beach Equine Clinic.
“When you are inside the joint with an arthroscopic camera, you have the most complete picture of the surface and health of that joint,” Dr. Davis noted.
Diarrhea can be a common problem for horse owners, but how do we know when it is serious? What are some of the causes? How do we treat severe cases and what potential complications you should watch for? Internal Medicine Specialist Dr. Peter Heidmann of Palm Beach Equine Clinic in Wellington, FL, has the answers to these questions and more.
Diarrhea, defined as loose stools, or excessive and overly-frequent defecation, occurs when the intestine does not complete absorption of electrolytes and water. Simple changes in feed, exposure to lush grass, or a bite of moldy hay can cause brief irritation of the bowel, giving a horse diarrhea for a day or two, but anything more than that could be from a variety of more serious causes. Bacteria, viruses, and toxins are all factors that can damage the lining of the bowel and lead to equine diarrhea and other complications.
Causes of Equine Diarrhea
The organisms that cause equine diarrhea are mostly bacteria –Salmonella and Clostridium difficile are among the most common. Clostridium difficile is associated with antibiotic use in both people and horses. While antibiotics are useful to kill bad bacteria, they can also kill good bacteria at the same time, upsetting the balance of flora in the body. If a horse goes on antibiotics for any reason, such as a wound or an infection, that can upset the good bacteria in the intestines and cause bad bacteria, such as Clostridium difficile, to grow.
Clostridium difficile can be found naturally in the environment. There are various types of Salmonella, most adapted to birds or to cattle or other livestock, so horses that are around livestock have a higher rate of becoming infected with that particular bacteria. Horses can also carry Salmonella and not have any symptoms, so they can pass it to each other. If the healthy flora in the horse’s body is thrown off by even a small change in diet, or something bigger like a colic episode, or antibiotics, then Salmonella can grow up in its place.
Another bacterial cause of equine diarrhea can be a disease called Potomac Horse Fever. A bacteria called Neorickettsia risticii, which is carried by snails and conveyed by flies like caddis flies, causes Potomac Horse Fever. For this reason, horses that live near rivers or streams can become infected. During warm weather months, caddis flies pick up the bacteria from the streams and can transfer the disease to nearby horses that accidentally eat the flies or larvae. There are hotbeds for Potomac Horse Fever throughout the U.S., including the Potomac basin where it was first described, as well as many parts of the East Coast, and areas of Oregon, northern California, and Montana.

A viral cause of equine diarrhea commonly seen is Coronavirus. This gastrointestinal virus shreds the intestinal lining and can cause horses to become very sick. The body has to reline the bowel, and it does so quickly, but it takes three to five days, during which the horse may have severe diarrhea and secondary infections.
“Coronavirus was thought for a long time to just be an opportunistic infection and that the virus would take advantage of the horse already being sick, but now it is more and more believed to be the cause of its own type of disease,” Dr. Heidmann stated. “Like all of these diseases, it causes damage to the lining of the bowel and supportive care must be used to help the horse heal. Unlike bacterial infections, however, you cannot directly treat the organism, since there aren’t appropriate drugs to directly treat coronavirus in horses.”
Outside of the infectious causes of equine diarrhea, there are mechanical causes, such as ingestion of sand, which can be a common problem in locations like South Florida. Sand is irritating to the lining of the bowel and can cause damage from its weight, as well as its abrasiveness. In general, sand is irritating enough that the body cannot retain the fluid that it needs in the intestines. As a result, it will cause secretory diarrhea where too much water is being lost. Clearing the sand usually solves the problem and the bowel is then able to reestablish a healthy lining.
A final cause of diarrhea in horses is toxins. Toxic plants, such as Oleander, can be fatal in large doses, but if ingested in small amounts, can be a severe irritant to the bowel. Other toxins that a horse can ingest in the environment, such as phosphate or insecticides, may also cause diarrhea.
Treatment for Equine Diarrhea
The single most important treatment for diarrhea, no matter the cause, is supportive care. Supportive care includes providing intravenous fluids to replace the fluids lost, providing protein in the form of plasma for the protein lost due to lack of absorption, as well as balancing electrolytes.

The next most important step is taking measures to either reestablish good flora within the gut or to remove the bad bacteria. In the past, a powdered charcoal was used, which is great for absorbing bacteria, but does not absorb the water. A gastrointestinal health supplement called BioSponge® came on the market in the early 2000s through the company Platinum Performance. The product is a purified clay powder that binds the toxins, and also binds the water, so that the horse loses fewer fluids in their equine diarrhea.
While absorbing the bad bacteria and toxins is important, also providing good bacteria in the form of probiotics can be very helpful.
“Probiotics are very variable in their efficacy, but there are some bacteria that are known to be associated with gut health,” Dr. Heidmann noted. “The good bacteria in people, and in horses, that has the most data for being helpful is Saccharomyces Boulardii. Old-fashioned brewers yeast is also Saccharomyces, but it is a different species, Saccharomyces cerevisiae.
“One of the best ways to re-establish healthy flora is Transfaunation, which is taking a healthy horses manure, filtering it, and then tubing it into the sick horse,” Dr. Heidmann added. “That is one of the most dramatic treatments out there. It provides the good ‘bugs’ that the horse is losing through the diarrhea. You will often see foals eating their mother’s manure. It is an instinctual habit to get the good bugs into their stomach. We only do that in the sickest of cases. Whatever the route, it makes a big difference to provide the good bugs because that creates the environment for the gut to heal.”
While some antibiotics are warranted in the right situation, Dr. Heidmann pointed out that they are not necessary as often as people would think.
“With people or dogs, if we get Salmonella or some other intestinal infection, we almost always go on antibiotics, but because antibiotics are the cause of many cases of colitis in horses, in general, that is not the best strategy,” Dr. Heidmann stated. “There are a couple of exceptions. Clostridium difficile does respond to antibiotics, metronidazole being the most common one. For Potomac Horse Fever, Tetracycline broad-spectrum antibiotics are the best.”
Biosecurity measures should also be taken to protect healthy horses from an infectious barn-mate. Dr. Heidmann recommends complete isolation of the sick horse while it is ill, and for a minimum of two full weeks after the infection has been clinically resolved. This includes no horse-to-horse contact, as well as no shared use of wheelbarrows, pitchforks, etc.
Molecular and DNA testing can be done to make sure that the horse is infection-free, however, Dr. Heidmann warns that testing can be problematic.
“There is a very high number of false negatives, meaning there is truly some infection there, but the lab cannot find it,” Dr. Heidmann stated. “There can be times when the horse is shedding bugs, but the tests do not pick it up. The state-of-the-art standard of care is a DNA test called ‘PCR’, and yet you still have to do multiple tests to get a positive test and get a diagnosis. Still, the best way to be safe is to continue testing until you are sure.”
Complications of Equine Diarrhea
Dr. Heidmann warned of common complications in severe diarrhea cases, laminitis being highest on the list. With the sickest of horses, it is unfortunately not uncommon for the veterinarian to get the gut fixed over three to five days, and then find that the feet have started to become very inflamed due to toxins in the bloodstream. If the horse loses the lining of its intestine, then the good and bad bacteria that are supposed to be contained in the intestine can “leak” out into the bloodstream and are free in the abdomen. Those bacteria are then dying either from an attack by the immune system or antibiotics, and they release endotoxins into the bloodstream, which along with other inflammatory products, can cause laminitis.
Another serious complication is blood clotting. The sick horse may become very low on blood protein when the bowel lining is damaged, which can cause clotting abnormalities. The horse may have difficulty clotting or they may become prone to abnormal increases in clotting. The horse might seem better, and then it will develop a clot somewhere in the body. It can be anywhere, but it is most often in the intestine itself, which is usually fatal. In general, horses like this are treated with supplemental protein in the form of plasma. In some cases, the veterinarian will also provide anticoagulant medications.

Although some cases of equine diarrhea are brief and easily resolved, Dr. Heidmann reminds that serious cases can go downhill fast, and it is important to refer to an expert.
“The biggest sign of a problem is duration,” Dr. Heidmann concluded. “If it is one day, it could be that they had a bite of bad food or something simple. If there are fevers or lethargy, those are instant warning signs. If it lasts for days, or if they go off their feed, those are instant warning signs. That is when you should call your veterinarian right away, especially because as they start to go downhill, these complications really amplify. The worst cases are the ones that have been smoldering for a day or two.”
Dr. Heidmann and the veterinarians at Palm Beach Equine Clinic are always available and encourage owners to contact the clinic at the first sign of a problem.
Palm Beach Equine Clinic, based in Wellington, FL, boasts one of the most advanced laboratory facilities in the country with onsite equipment capable of performing internal hematology, chemistry, and microbiology testing, as well as many regenerative therapies.
The facilities provide a plethora of services that are not only useful to Palm Beach Equine Clinic veterinarians, but also the many veterinarians who visit South Florida during the winter show jumping, dressage, and polo seasons.
Functions of the Palm Beach Equine Clinic Laboratory
Coupled with technologically advanced imaging services, state-of-the-art surgical capabilities, and care from renowned veterinarians, Palm Beach Equine Clinic takes pride in their onsite laboratory, which offers vital services to a range of clients providing rapid results.

Most commonly used, hematology is the study of blood, its chemistry, and components. A complete blood count or CBC determines the number and type of white and red blood cells circulating through the bloodstream. This can be quickly and easily performed in Palm Beach Equine Clinic onsite laboratory. Changes in these blood cells can indicate inflammation, infection, or disease. Quick diagnosis leads to more proactive and efficient treatment plans.
A clinical chemistry is the study of the chemical composition of a sample. Typically, the liquid portion of blood (either serum or plasma) is used for testing components such as electrolytes, kidney enzymes, and muscle enzymes. The serum or plasma is evaluated to determine the efficiency and health of specific organs.
Finally, microbiology is the study of small organisms such as bacteria, viruses, fungi, and other single-celled life forms. Hundreds of microbiology tests can be performed at Palm Beach Equine Clinic to look for signs of infection. The cultures are used to identify a specific bacteria or fungus present and sensitivity tests are used to determine which treatment, such as an antibiotic, will most effectively treat the infection.
For Palm Beach Equine Clinic veterinarian Dr. Samantha Miles, having an on-site laboratory with many different services enables her to provide faster and more affordable results to her clients and the horses in her care.
“We tend to get results so much faster in our own lab,” said Dr. Miles. “Also, an in-house culture is much less expensive than sending the sample away. It takes 24 hours to run a culture and 24 hours after that for the sensitivity. So usually it takes 48 hours to get a full culture and sensitivity, whereas to send that away you’re looking at least at 72 hours minimum and sometimes it’s a couple days longer than that.”
While laboratory technologies are common in determining a diagnosis and identifying different infections and viruses; they can also be used to more effectively and quickly treat common equine problems such as colic.
“There has been a lot of research lately comparing blood lactate to the abdominal fluid lactate, and the difference being a good indicator of whether a colic is surgical versus medically managed,” said Dr. Miles. “Sometimes it’s obvious, but not always so it is really helpful to have that capability. What we do is test a blood lactate sample using a lactometer, which takes about a minute. If a horse is dehydrated and has a higher lactate in the abdomen, we will rehydrate the horse and take it again. If the lactate value doesn’t decrease after rehydration we have a good indication that it is a real number and there is a surgical problem.”
Regenerative Therapies
According to Dr. Miles, some of the most impressive functions of the Palm Beach Equine Clinic laboratory include its regenerative therapy capabilities such as:
- Stem Cells
- Platelet-Rich Plasma (PRP)
- Interleukin-1 Receptor Antagonist Protein (IRAP)
- Pro-Stride Autologous Protein Solution (APS)
These can be applied to previously difficult to manage joint diseases and injuries using natural-occurring proteins, cells, and other natural processes originated from within the body of the horse. Essentially, these treatments use the horse’s own biological mechanisms to stimulate healing without the use of steroids or other drugs.

Stem cells are commonly derived from bone marrow which are cultured and multiplied into millions of stem cells. The cultured stem cells are injected into the affected tendon, ligament, or joint to encourage healing. PRP is another byproduct that is internally sourced from blood platelets in a matter of minutes. The platelets are combined with numerous growth factors that are released upon activation and can enhance healthy inflammatory cells in areas of tissue injury, form new blood vessels, new connective tissue, and aid in the regeneration of skin when injected.
IRAP, stands for Interleukin-1 Receptor Antagonist Protein, is used to treat equine athletes that are susceptible to musculoskeletal injuries and osteoarthritis or degenerative joint disease. Joint trauma results in the release of inflammatory mediators such as Interleukin-1 (IL-1). IRAP uses a horse’s own anti-inflammatory protein found within the blood to counteract the destructive effects of IL-1 to slow the process of osteoarthritis. The process works by binding to the IL-1 receptors in the joint and blocking the continuation of damage and inflammation.
“We often see joint damage in sport horses because of the nature of their work, but we try to avoid overuse of steroids in joints because steroids can have long term effects on cartilage,” said Dr. Miles. “This is a way we can manage joint disease and stop inflammation without having to consistently use steroids every time. Some of our clients will maintain their horses on IRAP alone for joint injections.”
Most recently, Palm Beach Equine Clinic has added a Pro-Stride Autologous Protein Solution (APS) Device, which is a new up and coming treatment that combines PRP and IRAP treatments but provides faster results.
Pro-Stride APS will reduce pain associated with arthritis and deliver anti-inflammatory proteins capable of slowing cartilage damage and improving mobility through the Interleukin-1 Receptor Antagonist Protein. The process can provide pain relief for up to one year following a single injection, which includes 20 minutes of blood processing in the Palm Beach Equine Clinic laboratory with no incubation period.
“I believe we are learning more about these technologies with more advanced science behind what they do and how they do it, “ said Dr. Miles. “These treatments are natural, drug-free, competition safe and necessity drives the need for regenerative therapies in the sport horse world.
“It’s all these new regenerative therapies that I think make our lab more state-of-the-art,” continued Dr. Miles. “They set us apart and are also tools that referring vets can make use of. The bottom line is that we have the ability to get horses back significantly faster after injury by using these therapies.”
An Expert Team
The laboratory at Palm Beach Equine Clinic offers 24-hour service with quick and efficient processing of blood work and test results. While veterinarians, or interns under the supervision of a veterinarian, are involved in a lot of the laboratory processing, the Palm Beach Equine Clinic laboratory is also staffed by 24-hour technicians. As a result, test results are returned to veterinarians and subsequently horse owners as fast as possible.
“We are lucky enough to have access to the technologies found in the Palm Beach Equine Clinic laboratory and work with people who have the experience, knowledge, and training to run such an advanced facility,” said Dr. Miles. “We always look forward to welcoming new and returning referring vets to the equipment, technology, and innovation that we have available at Palm Beach Equine Clinic. We take pride in our symbiotic relationship with veterinarians visiting Florida from around the country and the world.”
Palm Beach Equine Clinic of Wellington, FL, proudly offers advanced services to referring veterinarians and clients in equine podiatry with the expertise of Dr. Stephen O’Grady. As the show season continues on, some horses may be experiencing foot soreness or new lameness that could be related to their farriery.
The importance of high quality hoof care in the competition horse can’t be denied. The equine hoof is unique, as it is comprised of a group of biological structures that follow the laws of biomechanics (Figure 1). The farrier is a major asset during the show season as he or she can be proactive in maintaining the health of your horse’s feet and thus preventing lameness.

There are three very important aspects of farriery science that the farrier will use to keep your horse sound, which are trimming the foot in conjunction with the size and placement of the horseshoe. Typically, a farriery session will begin with an evaluation of the conformation of each hoof from the front, side, and behind to observe the height of the heels. Next, the farrier should observe the horse in motion to see whether the horse’s foot lands heel first, flat or toe first. All this information is considered and evaluated before the farrier begins shoeing.
Trim
Regarding the trim, many farriers no longer use the term ‘balance the foot’ – which has no meaning – and have begun to use guidelines or landmarks when approaching the trim. The guidelines used are trimming to achieve a straight hoof-pastern axis, using the widest part of the foot which correlates to the center of rotation, and trimming the palmar foot (heels) to the base of the frog or to the same plane as the frog (Figure 2, 3).
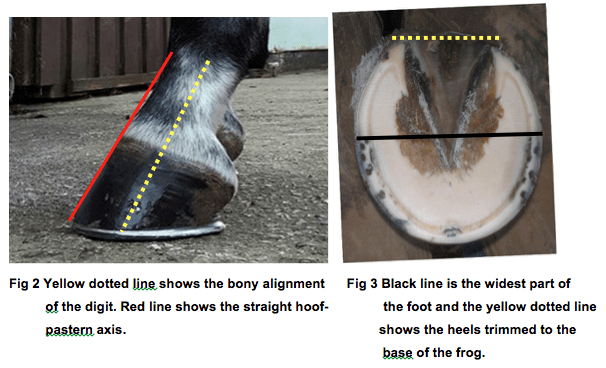
A closer look at these three guidelines, which are all interrelated, will help to show their importance. If the dorsal (front) surface of the pastern and the dorsal surface of the hoof are parallel or form a straight line, then the bones of the digit (P1, P2, P3) are in a straight line, and the force from the weight of the horse will go through the middle of the joint. Furthermore, and equally important, if the hoof-pastern axis is straight, the weight will be distributed evenly on the bottom of the foot.
The second guideline is the center of rotation (COR), and as the COR is located a few millimeters behind the widest part of each foot, it allows the farrier to apply appropriate biomechanics to each foot. The foot is trimmed in approximate proportions on either side of the widest part of the foot, which provides biomechanical efficiency.
Heels
Lastly, one should trim the palmar section of the foot to the base of the frog or trim such that the heels of the hoof capsule and the frog are on the same plane. Adherence to this guideline keeps the soft tissue structures (frog, digital cushion, ungula cartilages) within the hoof capsule, which are necessary to absorb concussion and dissipate the energy of impact.
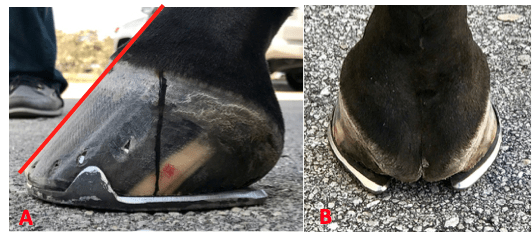
We must remember that heels do not grow tall, they grow forward. If we allow the heels to migrate forward, the soft tissue structures will be forced backward out of the hoof capsule. Furthermore, as the heels migrate forward, the weight is placed on the bone and lamellae, thus bypassing the soft tissue structures of the foot. Allowing the heels to migrate forward also decreases the ground surface of the foot. An example of this guideline is shown in Figures 4A & 4B, where the palmar foot was trimmed appropriately and a size larger shoe was applied to properly distribute the weight.

These three guidelines can be applied to any foot and they serve as a basis for maintaining a healthy foot and a basic starting point for applying farriery to a horse with poor foot conformation or one with a distorted hoof capsule. Figures 5A & 5B will illustrate a hoof where all three of these guidelines have been applied.
Farriery and Horse Showing
Many horses are given a rest from competition, which includes their feet, following a heavy competition load such as Wellington’s Winter Equestrian Festival and Adequan Global Dressage Festival. Many horses arrive with very reasonable foot conformation, but upon arrival the farriery can change and many horses are shod with various specialty shoes, wedges, pads, pour-ins, etc. as a means of protection, and perhaps, to enhance their performance.
As the season progresses and the workload increases, the sole thickness starts to decrease and the feet become softer from multiple baths; now the farriery that was applied for protection may be causing pressure on the thinner, softer structures of the foot, thus becoming somewhat detrimental. Furthermore, the horses continue to be trimmed and shod on a monthly basis and the change in the integrity of the hoof structures without investigating can cause horses to be over-trimmed. Additionally, as the season starts into March, the structures of the foot deteriorate further as a result of the workload, and many horses become foot sore. At this point, the farrier options are limited because they may have been used at the beginning of the season.
Luckily, Palm Beach Equine Clinic offers a farriery consultation service by Dr. Stephen O’Grady to both veterinarians and farriers. This unique service provides a second opinion or ‘another set of eyes’ to both professions when treating difficult farriery cases for ideas on other options to help these foot sore horses.
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. To find out more, please visit www.equineclinic.com or call 561-793-1599.
Palm Beach Equine Clinic (PBEC), located in Wellington, FL, offers advanced diagnostic imaging, world-renowned surgical talent, and state-of-the-art facilities necessary to quickly diagnose, treat, and repair horses with condylar fractures, making PBEC one of the leading facilities in the U.S. for condylar fracture repairs.

With thanks to the technology required for early diagnosis and experienced surgeons on staff, horses that are admitted to PBEC for condylar fracture repairs are more likely to return to training quickly. Most commonly seen in Thoroughbred racehorses and occasionally polo ponies or eventing horses, a condylar fracture was once considered a career-ending injury. Today, however, advances in technology aid in a full recovery with horses regularly returning to competition in their respective divisions.
What is a Condylar Fracture?
A condylar fracture is a repetitive strain injury that results in a fracture to the cannon bone above the fetlock due to large loads transmitted during high-speed exercise. On a radiograph, a condylar fracture appears as a crack that goes from the fetlock joint up the cannon bone. Lateral fractures many times exit the bone usually one-third of the way up the bone. Medial fractures will oftentimes spiral up to the hock or knee. Medial fractures are much more common in the hindlimb than the forelimb. It is the spiral fractures that are more difficult, due to the fact that the extent of the spiral cannot be identified radiographically. If the surgeon cannot identify the fracture, then that part of the fracture cannot be repaired.
“A condylar fracture is a disease of speed,” said Dr. Robert Brusie, a surgeon at PBEC who estimates that he repairs between 30 and 50 condylar fractures per year. “A fracture to the left lateral forelimb is most common in racehorses as they turn the track on a weakened bone and increased loading on the lateral condyle.”
Condylar fractures are further categorized into two classes. An incomplete and non-displaced fracture means that the bone fragment is not separated from the cannon and is still intact with its original position. A complete and displaced fracture means the fragment has detached from the cannon bone and this fracture can often be visible under the skin. Displaced condylar fractures have a somewhat lower prognosis due to the fact that soft tissue structures, such as the joint capsule, become torn. When these structures heal, they are thicker, which makes the joint less flexible.

“Most lateral condylar fractures are fairly simple for us to fix,” said PBEC surgeon Dr. Weston Davis. “Medial condylar fractures tend to be more complicated configurations because they often spiral up the leg. Those require more advanced imaging and more advanced techniques to fix.”
What is the Treatment?
The first step to effectively treating a condylar fracture through surgery is to accurately and quickly identify the problem. PBEC’s Board-Certified Radiologist Dr. Sarah Puchalski utilizes the advanced imaging services at PBEC to assist in the diagnosis.
“Stress remodeling can be detected early and easily on Nuclear Scintigraphy before the horse goes lame or even develops a fracture,” said Dr. Puchalski. “Early diagnosis of stress remodeling allows the horse to be removed from active race training and then return to full function earlier. Early diagnosis of an actual fracture allows for repair while the fracture is small and hopefully non-displaced.”
Once identified as a condylar fracture, PBEC surgeons step in to repair the fracture and start the horse on the road to recovery. Depending on surgeon preference, condylar fracture repairs can be performed with the horse under general anesthesia, or while standing under local anesthesia and sedation. During either process, surgical lag screws are used to reconnect the fractured condyle with the cannon bone.
“For a very simple and small non-displaced fracture, we would just put in one to two screws across the fracture,” explains Dr. Davis. “The technical term is to do it in ‘lag fashion’, such that we tighten the screws down heavily and compress the fracture line. Many times the fracture line is no longer visible in x-rays after it is surgically compressed. When you achieve good compression, the fractures heal very quickly and nicely.”
More complicated fractures, or fractures that are fully displaced, may require more screws to align parts of the bone. For the most severe cases of condylar fractures, a locking compression plate with screws is used to stabilize and repair the bone.
Severe condylar fractures often require general anesthesia, but for PBEC surgeon Dr. Jorge Gomez, approaching a simpler non-displaced condylar fracture while the horse is standing helps to aid in a faster recovery and successful surgical outcome.

“I think it takes the risk of anesthesia away and is a faster surgery from the time the horse comes in to the time the horse recovers,” said Dr. Gomez. “I will just sedate the horse and block above the site of the fracture. Amazingly, horses tolerate it really well, and it is very convenient for medial condylar fractures. In these cases, the fracture can spiral all the way up through the cannon bone, and they have a tendency to develop complete catastrophic fractures that can happen at any time after the injury. That risk can be significantly increased by the recovery from general anesthesia. Our goal is always to have the best result for the horse, trainers, and us, as veterinarians.”
According to Dr. Gomez, the recovery time required after a standing condylar fracture repair is only 90 days.
While Dr. Brusie, Dr. Davis, and Dr. Gomez are all seasoned in quickly and effectively repairing condylar fractures, PBEC is helping them to stay on the cutting edge of surgical techniques. PBEC is currently renovating its facility with plans to give surgeons a new approach to fix condylar fracture repairs. A set of stocks and surgeon’s pit have been added with the ability to give the surgeon eye-level access to the fracture with the patient standing and subsequently simplifying the procedure by reducing the risk from recumbent recovery.
What is the Prognosis?
One of the most common questions regarding an equine injury is, “Will the horse return to work?” Thanks to advanced imaging and surgical techniques, the answer to that question when involving a condylar fracture is most likely, “Yes.” At PBEC, a condylar fracture diagnosis rarely results in the end of a racehorse’s career.
Diagnostic imaging plays a major role in assisting to diagnose, surgically map, and follow up on condylar fractures. After primary use to diagnose a condylar fracture, digital radiographs are also used after surgery to ensure that a fracture repair was completely successful. According to Dr. Davis, scanning two planes during and after surgery gives a full view of the fracture and repair techniques, immediately indicating the success of the procedure before moving the horse on to recovery.
“A condylar fracture was once considered the death of racehorses, and as time and science progressed, it was considered career-ending,” said Dr. Brusie. “Currently, veterinary medical sciences are so advanced that we have had great success with condylar fracture patients returning to full work. Luckily, with today’s advanced rehabilitation services, time, and help from mother nature, many horses will come back from an injury like this.”
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. Make Palm Beach Equine Clinic a part of your team!
Palm Beach Equine Clinic of Wellington, FL, is a worldwide leader in sport horse medicine and emergency colic care. While symptoms of colic should be treated medically first, surgical intervention can be necessary, and the team at Palm Beach Equine Clinic is prepared for every situation.
With three Board-Certified Surgeons on staff, as well as a state-of-the-art hospital and the most advanced surgical equipment, Palm Beach Equine Clinic has a very high success rate in saving horses from life-threatening colic. The veterinarians take pride in their equine clients returning to full intended use and continuing to perform at their highest levels.

Causes and Symptoms
Colic is defined as any source of abdominal discomfort in the horse. Abdominal pain or problems within the gastrointestinal tract can arise unexpectedly from many different origins, including but not limited to: spoiled feed, abrupt changes in feed, parasite infestation, sand ingestion, lack of water consumption, excess stress, or changes in the weather. Many times there is not a well-defined inciting cause.
The most important step any owner can take is to recognize the symptoms as early as possible and immediately call their veterinarian. Pawing, rolling, looking at the abdomen, sweating, loss of interest in food and water, and absence of gut sounds in any of the four quadrants are common symptoms. The sooner the veterinarian gets involved in treatment, the better the horse’s chance of survival.
In the event of an emergency, the surgeons and veterinarians of Palm Beach Equine Clinic are available 24/7. When an equine patient is admitted to the hospital, every step is taken to quickly diagnose the problem and correct it immediately.
Tests and Diagnosis
Board-Certified Surgeon Dr. Weston Davis explained that one of the biggest challenges in the sport horse population is determining surgical versus non-surgical colic cases.
“We do not want to put a non-surgical case through the risk of anesthesia and the months of healing time, so we try to spare that at all costs and determine the surgical cases as accurately as we can,” Dr. Davis detailed. “On the split side of that, we try to operate as quickly as possible on any horse that needs surgery and not miss any surgical lesion types.”
There are several methods for differentiating surgical cases. Simple physical exam findings, such as the color of the gums, heart rate, gut sounds, and level of pain can all be supportive of surgical necessity. A variety of tests may also include abdominal ultrasounds and rectal exams.
An Abdominocentesis (or belly tap) is performed on every questionable colic case, where fluid is collected from around the intestines and analyzed for color and character. A variety of other laboratory tests will be run on the fluid as well, with the aim of quickly determining if the horse’s bowel is compromised.
Surgical Procedures
If surgery is necessary, there are a few different approaches that may be performed depending on the specific case.
For chronic colic cases, such horses with longstanding, intermittent colic, an abdominal exploratory procedure may be done with laparoscopy. This option can be done with the horse standing and is a minimally invasive way to examine the full abdomen.
In most acute cases, further steps must be taken. If the veterinarian determines that the horse is a surgical candidate, the patient will go under general anesthesia. The surgeons try to make as small of an incision as they can to perform the needed surgical correction.
“If we intervene early, we can take a strangulating or compromised lesion – one that most people understand as a twist – and we can go into the abdomen and correct the twist, reposition everything appropriately, explore the remainder of the abdomen to make sure nothing else is going on, and then close them up,” Dr. Davis explained. “Some of these surgeries can be as quick as 30 minutes and require just an untwisting, repositioning, and closure. The ones that are bad are the usually the cases that have a more severe twist or have been going on longer.”
In more severe or long-standing cases, the surgery can require a resection and an anastomosis procedure to excise a compromised or devitalized segment of the intestine. The surgeon then joins the healthy ends back together.
“Even more advanced procedures would be like a re-plumbing of the intestines,” Dr. Davis noted. “One of the most common examples of this would be a patient with damage to the end of the small intestine, near or involving its junction with the cecum. In a case like this, we would perform a ‘jejunocestomy’ where we join another part of the small intestine to a different position on the cecum.”
Post-Operative Recovery
After any surgery, there is a process of recovery, which Palm Beach Equine Clinic makes as easy as possible for its clients. In the traditional recovery, most horses will remain in the hospital for a few days. In the post-operative period, they generally receive fluids until they are ready to eat and drink, 3-5 days of antibiotics, and 5-7 days of anti-inflammatories.
“The recovery process is highly dependent upon how sick they are after surgery,” Dr. Davis stated. “Some horses will bounce back and be home 48 hours later, but a very sick horse could potentially spend seven to ten days in the hospital until they are healthy enough to get off fluids and go home.”
After leaving the hospital, the horse is usually placed on one month of stall rest, followed by another month of turnout in a small paddock. In between eight to 12 weeks, the horse will usually be fully recovered and ready to start back to work.

Physical Therapy
With the sport horse in mind, PBEC pays special attention to the health of the abdomen following surgery. The health of the abdominal incision and prevention of infection or hernias is very important. In most cases, the surgeon will recommend physical therapy and special exercises to re-strengthen the horse’s abdominal muscles so that it can get back to work quickly and have a strong abdominal musculature when it does.
“Making the horse walk backwards is one thing that will make them tighten and work their abdominal musculature,” Dr. Davis shared. “Pinching or tickling around their tail head is another common exercise to make them do something similar to a stomach crunch.”
As one of the top equine emergency care centers in the world, Palm Beach Equine Clinic is prepared to handle any case, 24 hours a day, seven days a week, and 365 days a year.
“With the combination of quick surgical intervention, excellent surgical care, and specialized post-operative measures, Palm Beach Equine Clinic has a very high rate of return to athletic performance for all of our colic cases,” Dr. Davis concluded.
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. To find out more, please visit www.equineclinic.com or call 561-793-1599.
Several regions across the U.S. have reached the peak of the winter show season, and with the increase in equine travel, as well as large populations of horses in close contact with one another, proper vaccination protocols are as important as ever.
Dr. Kathleen Timmins of Palm Beach Equine Clinic in Wellington, FL, is often asked why proper equine vaccination protocols are imperative for all horses, and her answer voices directly to the welfare of the horse.
“You could save your horse’s life!” she said. “It is really important from an infectious disease standpoint, but also for mosquito-borne diseases or rabies; these are diseases that are life-threatening for lack of a $25 vaccine.”
Vaccinations: When, What, and How
According to Dr. Timmins, recommended vaccination protocols vary by vaccine and by the location of the horse, but the core group of vaccines is relatively standardized. As a rule, horses should receive vaccines to prevent mosquito-borne diseases like Eastern Equine Encephalitis (EEE), Western Equine Encephalitis (WEE), and West Nile Virus twice a year. Equine Encephalitis is characterized by the swelling of the brain in an infected horse, while West Nile Virus infects the central nervous system and may cause signs of Encephalitis, including those ranging from fever to weakness and paralysis of the hind limbs.
“Vaccinations against mosquito-borne diseases become very important in south Florida because we have mosquitoes year-round,” said Dr. Timmins. “As you go further north, owners may sometimes choose to only vaccinate against those once a year.”
Included in the twice-a-year vaccination program is a Flu/Rhino dose. Flu vaccination prevents the illness in horses much the same way it does in humans, while the Rhino vaccine is key in helping to prevent the Equine Herpesvirus (Rhinopneumonitis). Equine herpesvirus type 1 (EHV-1) and Equine herpesvirus type 4 (EHV-4) most commonly result in respiratory disease in horses and can progress to neurological disease.
East and West Equine Encephalitis, West Nile, and Flu/Rhino can all be administered as a combination vaccine requiring only one injection.
In addition to vaccinations given twice a year, annual vaccinations include those to prevent Potomac horse fever, a potentially fatal illness that affects the digestive system and is caused by the intracellular bacterium Neorickettsia risticii; Strangles, a bacterial infection of the upper respiratory tract; and Tetanus, an acute, often fatal disease caused by the bacteria Clostridium tetani found in soil.
Much like the vaccinations administered to humans, the companies that produce the vaccines are in constant transition, adapting each vaccine to the most common strains to ensure the most accurate prevention of disease.
The Role of the Horse Show

To combat the rise of infectious disease outbreaks, many horse show organizers have taken a proactive step to reduce the spread of disease by developing vaccination requirements for the show grounds. This is a step towards preventing disease as an organized community, according to Dr. Timmins.
“No one wants sick horses,” she said. “All horse show organizers can do is put the requirements out there and hope that people comply and that they understand why vaccinations are so important.
“When a horse pops with a fever at a show everyone is alarmed,” continued Dr. Timmins. “If proper vaccination protocols are followed, it is easier for us to figure out why that horse has a fever and treat them quickly and appropriately.”
Negative Reactions
There are occasional cases of horses reacting negatively to certain vaccinations, making a regular schedule difficult. After receiving a vaccine intramuscularly, some horses experience local muscular swelling and soreness or signs including fever, anorexia, and lethargy. Severe reactions such as anaphylaxis can also occur in rare, extreme cases.
According to Dr. Timmins, there are procedures in place to help keep horses that suffer reactions on a systematic vaccination plan without threatening their health or competition schedules.
“What I will do first is break up the vaccinations so we can figure out which one is bothering the horse,” said Dr. Timmins. “Then sometimes all it takes is a change in the vaccine company because the particular horse is reacting to their preservative or their carrier. Veterinarians can also pretreat with a nonsteroidal anti-inflammatory drug to avoid really bad reactions. Finally, there is always an option to administer intranasal vaccines rather than using an injectable.
“Very few horses have severe reactions to vaccines and for the most part, the horses traveling to shows are part of a young and healthy populations,” continued Dr. Timmins.
As the winter horse show season continues throughout the U.S., horse health must be a priority and vaccinations are a simple way for the equine community to do their part.
“Vaccinations are an easy and relatively inexpensive way to prevent infectious disease outbreaks, and keep our horses healthy and safe,” she said. “There’s just no reason not to vaccinate.”
More About Dr. Timmins

Dr. Kathleen A. Timmins is a 1993 graduate of the Ohio State University School of Veterinary Medicine. She completed her internship in equine medicine and surgery at the Illinois Equine Hospital near Chicago. Prior to coming to Florida, Dr. Timmins practiced in Aiken, South Carolina, where she met her husband, John, who plays polo professionally. Growing up in Central Ohio, Dr. Timmins began her relationship with horses as a child on the hunter/jumper circuit. She continues to ride and show as much as possible. She and her husband are enjoying parenthood with their daughter Schuyler.
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. Make Palm Beach Equine Clinic a part of your team by calling 561-793-1599.

Palm Beach Equine Clinic of Wellington, FL, has a team of over 30 skilled veterinarians, including three Board-Certified Surgeons, one of the world’s only Board-Certified equine Radiologists, and numerous other experts in their fields. Palm Beach Equine Clinic’s surgical team leader, Dr. Robert Brusie, is a nationally renowned Board-Certified surgeon whose surgical specialties include orthopedic, arthroscopic, and emergency cases. Dr. Brusie has been the head surgeon with Palm Beach Equine Clinic for the past 20 years and is a beloved part of the team.
Dr. Brusie graduated from Michigan State University College of Veterinary Medicine. He completed his surgical residency at the Marion DuPont Scott Equine Center in 1989 and has been in private practice ever since. He became a Diplomate of the American College of Veterinary Surgeons in 1994. Dr. Brusie joined Palm Beach Equine Clinic in 1996.
Dr. Brusie is a Board-Certified Surgeon who is recognized for his expertise in colic surgery, as well as for his skill in arthroscopic surgery. His surgical experience expands the clinic’s progressive care in both emergency and elective procedures. He has published articles on numerous topics, including the equine intestinal tract and septic arthritis in horses. Dr. Brusie is married and has three daughters.
What was your background with horses growing up?
I grew up on a farm in Michigan. We had usually between 200-600 head of cattle and always between four to six horses. Our horses were cow ponies or driving horses. My dad loved horses and had to have them around. My family has owned our farm for six generations – it pretty much occupied all of our time besides sports and school. Needless to say, we didn’t have much time to show horses.
When and why did you decide to become a veterinarian? Did you know you wanted to be a surgeon from the start?
I decided to become a veterinarian at an early age. I think I was seven or eight years old when I pulled my first calf. One of my dad’s hired men called me ‘doc’ when I was about that age. When I went to college, my plan was to become a large animal veterinarian and live in my hometown and continue to farm part-time with my three brothers. All of that changed when I was in Veterinary school at Michigan State University. Dr. Ed Scott was one of the five surgeons at MSU. He was a gifted surgeon and a great teacher. He kind of steered me into an equine internship at Auburn University. It was one of those things that the more you did, the more you wanted to do to improve yourself. I operated my first colic by myself when I was three weeks out of vet school (32 years ago).
How did you first start working at Palm Beach Equine Clinic?

I was a surgeon at a clinic in Atlanta. In 1996 I had performed surgery for a client of Dr. Paul Wollenman’s. He had started this practice in 1975. He asked me if I needed a job. I was planning on staying in Atlanta for the rest of my career. I received phone calls from the other two partners over the next nine months, and eventually with encouragement from my fiancé, now wife Melissa, I took the job.
What do you love most about working at Palm Beach Equine Clinic?
We have an exceptional group of veterinarians and staff here. The depth and scope of our veterinarians is amazing due to the large caseload. On any individual case, there may be two to three doctors that have input on the case to ensure no stone is left unturned.
Additionally, we are so privileged to work on some of the best show, race, and polo horses in the world. It is truly an honor.
What sets the surgical services at Palm Beach Equine Clinic apart?
Between Drs. Gomez, Davis, and myself, we perform just about every soft tissue and orthopedic surgeries that are done in our field.
Personally, my greatest sense of success is when I see a horse back after surgery going as good or better than it was prior to surgery.
What are the biggest changes you have seen in sport horse medicine over the years?
Currently, the most exciting thing we see going on in medicine is regenerative therapy. Twelve to 15 years ago, we were harvesting bone marrow from the sternum and injecting it into lesions in tendons and ligaments. Now we manipulate the bone marrow or other sources of stem cells to promote more rapid and more functional healing of some of these injuries. I can assure you that in 10-20 years what we are doing now will seem stone-aged by then. There are some very clever minds performing some serious research in this field.
How do you stay up-to-date on new medical advances?
Every veterinarian at Palm Beach Equine Clinic tries to attend as many meetings as time allows. We also do a weekly journal club at our clinic to discuss recently published papers in veterinary and human medicine and surgery.
What is the most interesting or challenging surgery that you have done?
Dr. Gomez and I had a three-year-old racehorse that had split his P1 (long pastern bone) and cannon bone in the same leg in a race. We were able to piece together both bones perfectly and the horse recovered brilliantly. He probably could have returned to racing, however, the owners elected to retire him to life as a breeding sire.

How do you spend your free time when you are not working?
When I’m not doing something with my family, I really enjoy woodworking. My current project is building a kitchen table for Sarah, my assistant of 12 years. In the summer, I get roped into helping on my brother’s farm.
What is something interesting that people may not know about you?
I have three daughters who I am very proud of and tend to brag on maybe a little too much. My oldest, who was a nationally ranked swimmer, is now an anesthesiologist in human medicine. My middle one is either number four or five (depending on the week) in the nation in debate, and my youngest will probably run the free world (you will have to ask her if she wants to).
How else is the family involved in horses?
My wife (Melissa) and youngest daughter (Kayla) are horse nuts in the true sense of the word. Anything to do with horses (especially show hunters) they are dialed in. Melissa loves riding, and Kayla shows in hunters and equitation.
What makes Palm Beach Equine Clinic a special place for you?
I am blessed to have three good men as business partners. They are my good friends and great people. We are very lucky to have 20-plus veterinarians working with us who are very knowledgeable and caring individuals. We feel like a little practice, but with a lot of people who just get the job done.
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. Make Palm Beach Equine Clinic a part of your team!
Palm Beach Equine Clinic in Wellington, FL, has state-of-the-art surgical and advanced diagnostic imaging equipment available. With board-certified Radiologist Dr. Sarah Puchalski, Palm Beach Equine Clinic uses the Equine Standing Magnetic Resonance Imaging (MRI) and a Nuclear Scintigraphy (bone scan) camera to quickly and accurately diagnose injuries for their clients.
Every horse owner dreads seeing signs of lameness or discomfort in any horse, whether it is a backyard companion or a top-caliber sport horse. For performance horses, however, one of the first questions many owners ask upon contacting a veterinarian about a problem is, ‘Can the horse safely and comfortably return to work?’ Using Palm Beach Equine Clinic’s cutting-edge technology, Dr. Puchalski can quickly and accurately answer that question.

The Equine Standing MRI produces highly detailed images in several different planes to capture a complete image of a desired area. An MRI is best used to further define a specific area of both bony or soft tissue that has been pinpointed as the origin of lameness. The process can be completed while the horse is in a standing position and requires only light sedation.
Similarly, the process of Nuclear Scintigraphy (bone scan) begins with the injection of a radioactive isotope, specifically named Technetium 99. The isotope attaches to the phosphorous proteins localized within the bone and is absorbed over a few hours’ time. A specialized nuclear isotope gamma ray camera is used to capture images of the skeletal anatomy with a 360-degree view. Points of interest “light up” on the image to indicate increased metabolic activity and the site of injury.
Lameness or performance problems are most frequently approached through routine x-rays and ultrasounds, which can appear normal. Thus, it is difficult to diagnose subtle problems because the most common tools are not sensitive enough to diagnose in every case. At PBEC, the Equine Standing MRI and Nuclear Scintigraphy equip veterinarians with an advantage when troubleshooting a lameness issue and helps them to determine a correct, quick diagnosis.
Coupled with advanced technology, Palm Beach Equine Clinic is also one of very few equine practices in the U.S. with a Board Certified Radiologist on staff, and thanks to Dr. Puchalski, hundreds of MRI and bone scans are read each year at Palm Beach Eqine Clinic. In addition to state-of-the art diagnostic tools, the technology also affords economic benefits to owners.
“MRIs can give a definitive diagnosis, and that saves time and money in the long run,” said Dr. Puchalski. “For example, if a horse goes lame and is examined and treated empirically, which is a diagnosis based on likely problems through common diagnostic procedures, it either stays sound or it becomes lame again or even non-functional in three to six months. This method sets back the commencement of the appropriate therapy.

“What the MRI does is allow the horse to be treated early and correctly,” continued Dr. Puchalski. “Otherwise, you may not be treating the correct issue, and the horse could end up lame again very soon.”
Nuclear Scintigraphy does not produce a scan that is as specific, but it gives Dr. Puchalski the opportunity to procure a concrete quick diagnosis, as well as evaluate the whole horse for secondary problems.
“Oftentimes the primary problem in one place is making a horse sore in other places,” she said. “Owners like to know the root problem, but to also quickly diagnose secondary problems so the entire horse can be treated at once.”
As the official veterinary hospital of the Winter Equestrian Festival (WEF) and the Adequan® Global Dressage Festival (AGDF), Palm Beach Equine Clinic sees a high concentration of sport horses in need of care. In turn, owners of those horses are eager to see their horses quickly and happily return to competition.
“The biggest benefit to Palm Beach Equine Clinic and the Wellington community as a result of these MRI and Nuclear Scintigraphy scans is accessibility,” concluded Puchalski. “Anyone can call from the horse show to the clinic, get a scan scheduled quickly- in and out, get results fast, and then their training program can be changed immediately.”
About Dr. Sarah Puchalski
Dr. Sarah Puchalski is from Davis, CA, where she was an associate professor at the University of California in their Department of Surgical and Radiological Sciences. In 1995, she received her BS in biology from Simon Fraser University in British Columbia, and in 1999 earned her Doctor of Veterinary Medicine from the University of Saskatchewan in Saskatoon, where she received the ACVS Outstanding Large Animal Surgery Student award that same year. Dr. Puchalski interned in Field Service and Sports Medicine at New Bolton Center at the University of Pennsylvania in 2001, and completed her residency in radiology at UC Davis in 2005.
Dr. Puchalski has devoted her career to teaching and improving equine health through the development and refinement of diagnostic techniques. In 2011, she contributed to two books on the topic of equine lameness. Her recent contributions include chapters in “Diagnosis and Management of Lameness in the Horse,” edited by Ross and Dyson, as well as in “Veterinary Computed Tomography and the Clinical Veterinary Advisor: The Horse, Equine Colic and Veterinary Clinics of North America.” She also has contributed close to 50 scientific articles concerning the diagnosis of equine lameness to many periodic journals, including Veterinary Radiology & Ultrasound: the official journal of the American College of Veterinary Radiology and the International Veterinary Radiology Association; Veterinary Pathology; Equine Veterinary Journal; the American Journal of Veterinary Research; Equine Veterinary Education; Journal of the American Veterinary Medical Association; and Journal of Veterinary Internal Medicine.
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. Make Palm Beach Equine Clinic a part of your team!
Palm Beach Equine Clinic is proud to serve as the local headquarters for emergency services and equine diagnostics during the winter show season in Wellington, FL. As the official veterinary hospital of the Winter Equestrian Festival (WEF) and the Adequan® Global Dressage Festival (AGDF), Palm Beach Equine Clinic has been the premier surgical facility in Wellington for over three decades.
While competing in South Florida, horses and riders from around the globe have access to Palm Beach Equine Clinic’s state-of-the-art hospital for all of their sport horse needs. Palm Beach Equine Clinic has a team of over 30 veterinarians, which includes three Board-Certified Surgeons, a Board-Certified equine Radiologist, and numerous other experts in their fields. All competitors and their traveling veterinarians are welcome for the support of services and collaboration throughout the season.
Referral Veterinarians Welcome
The referring relationship between veterinarians is most commonly seen in the specialty departments of surgery, internal medicine, ophthalmology, and advanced diagnostic imaging. At Palm Beach Equine Clinic, the advanced diagnostic imaging and surgical technology is unmatched, and the three Board-Certified Surgeons are skilled in many procedures that require high levels of expertise and advanced current equipment. As a result, many veterinarians refer their clients to the facility for specialty services.
Dr. Weston Davis, one of the Board-Certified Surgeons on the staff at Palm Beach Equine Clinic, works with many referral cases. Throughout the year, veterinarians from all over Florida frequently refer their clients to Palm Beach Equine Clinic for surgical procedures and advanced diagnostic imaging. The referring veterinarians may range anywhere from general practitioners to other surgeons that do not have access to surgical facilities or the most modern diagnostic imaging modalities while on the road.
“As a rule, we are friendly with referring doctors and take care of their clients with as much high-level care and professionalism as possible,” Dr. Davis stated. “It is important to us to maintain good relationships with the veterinarians that refer to us for specialty work. We always try to facilitate whatever level of involvement they desire. If they want to come and be there for the surgical procedure, we make that happen, and if they just want to send the case and not be as involved, we can do that as well. However, we also always collaborate with the referring veterinarian and the client as a team. If they send a horse in for a surgical procedure, we are going to do the procedure and then connect the client with the referring physician for the follow-up.”

Talented Surgeons and Advanced Diagnostic Imaging
The cutting-edge services available at Palm Beach Equine Clinic are made possible by the expertise of the hospital’s talented surgeons, along with the assistance of state-of-the-art diagnostic imaging and comprehensive surgical and medical resources. The combination brings many of the best veterinarians in the world to Palm Beach Equine Clinic for assistance with their most complex cases.
Among the hospital’s features, the latest in surgical technology enables less invasive operations that result in faster recovery times for the horse. Dr. Davis explained how diagnostic imaging is used during surgery to help guide procedures and assure the best possible result.
“Magnetic Resonance Imaging (MRI) and other advanced diagnostic imaging modalities can often be used for three-dimensional mapping to help enhance the surgical technique,” he noted. “There are some fractures in particular where the surgeon can map out the exact configuration of the fracture off of the MRI scan. We are then able to place markers with the MRI to guide a more exact, refined surgery.
“Intra-operatively, x-rays are taken to view progress, particularly for fracture repairs,” Dr. Davis continued. “The digital radiographs allows us to view the fracture in two planes to ensure optimal screw placement and fracture repair. Ultrasound is also frequently used in surgery for some of the more delicate procedures, specifically with soft tissue.”
Other surgical procedures may be guided with Arthroscopy, which aids in visualization of a joint; Laparoscopy, which uses a camera inserted into the abdomen; or Endoscopy, which is used in upper airway procedures. With the most advanced diagnostic imaging technology onsite, Palm Beach Equine Clinic is the go-to hospital for equine owners and referral veterinarians from around the world during the winter season in Wellington.
Palm Beach Equine Clinic provides experience, knowledge, availability, and the very best care for its clients. Make Palm Beach Equine Clinic a part of your team! To find out more, please call 561-793-1599.




